Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/grjp.2020.110003Article Views : 176Article Downloads : 134
Always Carefully Evaluate the Atlanto-Axial Rotatory Subluxation in Children. One Case Report Presentation
Tiziana Greggi*, Luca Boriani, Antonio Scarale, Konstantios Martikos, Francesco Vommaro, Giovanni Ciani, Lucrezia Leggi, Milva Battaglia, Chiara Ghizzi, Mino Zucchelli
IRCCS: Rizzoli Ortopedic Institute Bologna Italy
*Corresponding Author: Tiziana Greggi, IRCCS: Rizzoli Ortopedic Institute Bologna Italy, Email: tiziana.greggi@ior.it
Article Information
Aritcle Type: Case Report
Citation: Tiziana Greggi, Luca Boriani, Antonio Scarale, et al. 2020. Always Carefully Evaluate the Atlanto-Axial Rotatory Subluxation in Children. One Case Report Presentation. Glob Res J Pediatri. 2: 06-13.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2020; Tiziana Greggi
Publication history:
Received date: 15 December, 2020Accepted date: 23 December, 2020
Published date: 26 December, 2020
Abstract
Background: Atlanta-Axial Rotatory Subluxation is an acquired condition, usually occurring in paediatric patients, because of either trauma or pharyngitis or ear-nose-throat (ENT) surgery or upper respiratory tract infection. Post-traumatic C1-C2 rotational subluxation in paediatric age is a very frequent event. It mimics benign torticollis but may result in permanent disability. The Atlanta-axial rotatory displacement, as defined initially by Fielding and Hawkins in 1977, is classified into four types: Type 1 is the most common form in children. It is a simple rotatory displacement without an anterior shift. Type 2 is potentially more dangerous. It is a rotatory displacement with an anterior shift of 5 mm or less. Type 3 is rotatory displacement with an anterior shift greater than 5 mm. Finally, type 4 is rotatory displacement with a posterior shift. Type 3 and 4 deformities are rare, but neurological involvement or even instant death may follow [Figure. 4] [18]. The condition requires prompt diagnosis by thorough examination to avoid any treatment delays. The difficulties for a timely and correct diagnosis and then the correct treatment is described.
Case presentation: A 5-year-old girl comes to the emergency room with cervical pain and stiffness. This painful state, as mum reports, has been lasted for about ten days, after a mild trauma. The radiographic picture demonstrates a rotary subluxation C1-C2, type 1 according to Fielding and Hawkins classification. The treatment is head-halter traction with 2kg, and nonsteroidal anti-inflammatory drugs (NSAIDs). After 2 days the x-ray picture improves, but the painful symptoms persist. An in-depth diagnostic MRI of the cervical spine and brain revealed a medulloblastoma which made an immediate and effective neurosurgical intervention necessary.
Conclusions: the C1-C2 rotatory dislocation must always be evaluated with extreme care, without neglecting any clinical and anamnestic information for a correct and timely differential diagnosis. Remember that children show very clearly what they feel, always.
Keywords: AARS; Cervical spine dislocation; Rotatory subluxation; Differential diagnosis; Medulloblastoma
Background
Under the pressure of the breaching time and busy shifts, many patients complaining of a sore or stiff neck and lateral flexion of the neck with contralateral rotation are discharged from the emergency department to the care of their general practitioners without adequate investigations. While most of the cases are due to benign causes, torticollis can be due to many congenital and acquired pathologies, some of which may need further investigation and urgent management. Rotational cervical dislocations due to congenital abnormalities are not very frequently reported [1,2,6]. As in the case of our little girl, congenital anomalies can be excluded c by simple x-rays. Anamnesis is important to consider or not a post-traumatic injury. Nevertheless, in some occasion’s anamnesis do not provide us with the certainty of an effective trauma, especially in children. Initial evaluation in AARS should be focused on eliminating inflammatory conditions or trauma as underlying causes. It is very important, for the purpose of treatment, to understand if it is an acute or chronic case. For acute cases, non-surgical management can be employed to treat the torticollis, beginning with the use of a cervical collar and analgesics [5]. Nontraumatic rotatory subluxation was first described by Charles Bell in 1830, in a patient with syphilis and pharyngitis who developed compression of the spinal cord and died. It was defined by Grisel as a syndrome in 1951 after the report of two cases of nontraumatic atlantoaxial rotatory subluxation with a recent history of pharyngitis. [1,2,6,16,17]. Grisel syndrome refers to atlantoaxial rotatory subluxation not triggered by trauma, affecting patients with a history of head and/or neck infections or occurring after otorhinolaryngology procedures [1]. It is a rare syndrome predominantly occurring in paediatric patients the diagnosis is established by the association of clinical and radiologic findings [15,17,19,21].
Case Presentation
History and physical Examination
A 5-year-old girl is brought to the emergency room by her mother for neck pain. The child presented with torticollis and resisted any attempt to move the head because of pain. The head was tilted to one side and rotated to the opposite side with the neck slightly flexed (a typical ‘cock robin’ position of the head) with associated muscle spasm of the sternocleidomastoid muscle. She had no neurological problems, no difficulties in walking and running. The mother at the reception in the emergency room was very anxious and reported anamnestic information’s in a contradictory way. She told that the little girl had cervical pain and stiffness since about 10 days, and that she had had a trauma, playing with her brother, many weeks before. The mother described the girl as particularly emotional, who often had morning headaches, even in the past. After two days in hospital, she informed us that the girl often had headaches and dizziness when she fidgeted, and had never had a perfect balance during her walking. During the third day, after further careful interviews by the ward doctor, the mother said what she denied at the entrance: frequent inflammations of the upper airways and a punch in the neck received by the child from her brother.
Management
After examining her with standard and AP open-mouth odontoid x-ray of the cervical spine, we admitted her with a diagnosis of C1C2 rotary dislocation. She was hospitalised for insights and chin traction for AARS. Not neurological Problems Were seen, except sometimes difficult in walking in a straight line.we decied to also MRI of the brain and spine.
Radiologic Finding
X ray of the cervical spine in anteroom posterior and lateral view plus the transoral projection, showed a contracted cervical spine, with the neck deviated to the left and the head turned to the right (cock robin position) with a minimum dislocation “ad latus” of the dens with respect to the lateral masses of C1, at the time of the first observation in the emergency room [Figure 1a,b]. Cervical CT scan performed after 2 days of traction showed a very small rotation of the C1C2 articular facets, without any anterior translation of C1 with respect to the tooth of the epistrophe [Figure 2a-2C]. Cervical and brain MRI did not show any cervical lesion, but showed a massive lesion of the cerebellar left hemisphere with peri-lesional tissue edema. Through the MRI we could also see mass effect on the IV ventricle and consequent Chiari I. These were clear signs compatible with cerebellar-hemispheric medulloblastoma associated with supratentorial hydrocephalus [Figure 3a-3c].

Figures 1: 1A_Initial anteroposterior radiograph of the cervical spine indicated loss of symmetry between lateral masses of the atlas and odontoid process. 1B_Lateral cervical spine radiograph showed loss of the normal lordosis.
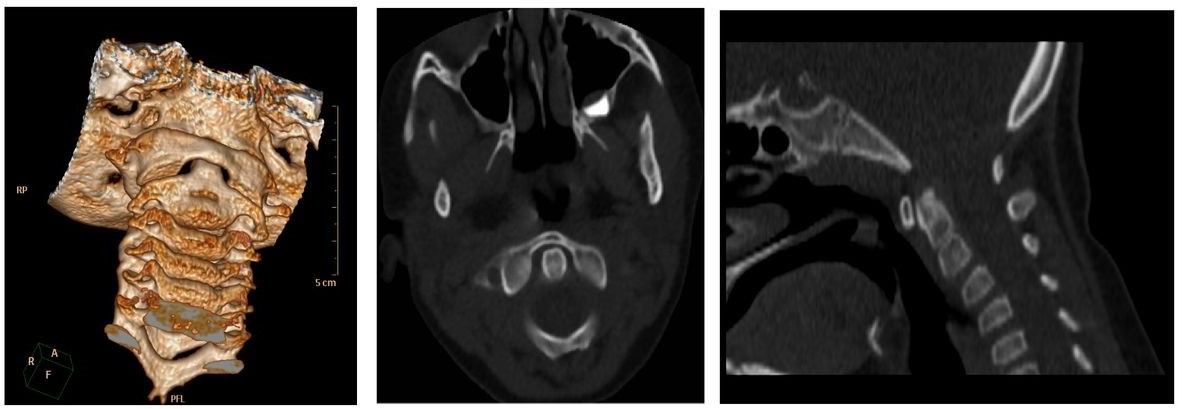
Figures 2: 2A_Coronal CT 3D images demonstrated narrowing of the left lateral atlantodental interval and a wider right lateral atlantodental interval. 2B._Axial CT views confirmed that the odontoid was lying eccentrically between the lateral masses of the atlas. 2C Sagittal CT views of the cervical spine indicated no abnormal findings.

Figures 3: 3A & 3B_left cerebellar hemisphere lesion + perilesional tissue edema. 3C_mass effect on the IV ventricle and Chiari I secondary signs compatible with cerebellar hemispheric medulloblastoma associated with supratentorial hydrocephalus.

Figures 4: Fielding Classification of AARD.
Dyagnosis and Surigal Treatment
After MRI the diagnosis of a cerebellar neoplasia was made, so we transferred the child to the paediatric neurosurgery department. Craniotomy was performed, and extemporaneous histological examination had a report of: medulloblastoma. The excision of the mass was performed with an ultrasonic aspirator, then plastic of the dura, repositioning and bone synthesis was performed. Post-operative recovery was excellent, without any neurological damage and with complete regression of symptoms. The definitive histological e examination was: nodular desmoplastic medulloblastoma (gr 4, WHO classification) [4]. She was therefore taken in charge by paediatric onco-haematology for adjuvant treatments.
Dissusion and Conclusion
In our case, clinical and laboratory tests were not indicative for Grisel syndrome: no significant blood tests, no inflammation, minimal increase in alkaline phosphatase and anti-streptolysin title. Radiographic examinations revealed a first-degree rotary dislocation. In an attempt to reach a diagnosis, we also considered that AARS may be also present in Sandifer syndrome which is characterized by spasmodic posturing of the neck, back, or upper extremities associated with gastroesophageal reflux, esophagitis or a hiatal hernia. We considered in differential diagnosis that AARS has been described in patients with autoimmune disorders, including juvenile idiopathic arthritis, ulcerative colitis, and HLA-B27-positive seronegative spondyloarthropathy [2,3,17]. In our case we had no evidence of these pathologies. Not to be overlooked in differential diagnosis as well is Bow hunter's syndrome (BHS). It is rare cause of vertebrobasilar insufficiency that arises from mechanical compression of the vertebral artery by head rotation, severe vertigo, dizziness, right upper extremity tingling sensations and aggravated syncope when she turned her head. Our little patient had some BHS symptoms such as dizziness, vertigo, but she did not have blurred vision when turning the neck [8,11,12]. Differential diagnosis with tumours should be considered, even if it is the least frequent cause of AARS. Brain tumours are the most common cancer in children < 15 years of age and are the 2nd leading cause of cancer-related childhood death. Diagnosis is generally based on radiological tests (usually MRI) and biopsy [2,15,19,20,22]. Treatment may include surgical resection, chemotherapy and radiotherapy. Medulloblastoma is the most common malignant brain tumour in childhood. The peak incidence occurs in children aged between 2 and 7 years. The neoplasm is very rare in the adult population (over 21 years). This tumour is typical of the posterior cranial fossa, where it is located in both hemispheres of the cerebellum or in the cerebellar worm and being invasive and rapidly growing it usually spreads to other parts of the central nervous system (CNS) through the CSF: it can infiltrate the floor of the near fourth ventricle and extend into its cavity. It can also pass into the meninges. More rarely, it can give extra CNS metastases. Symptoms at the onset of neoplasia include loss of balance, lack of coordination, diplopia, dysarthria and, due to the involvement of the fourth ventricle (for which an obstructive hydrocephalus is common), signs of hydrocephalus, including headache, nausea, vomiting, unstable gait [10,22]. Treatment is based on a combination of surgery, radiation therapy and chemotherapy. Magnetic resonance imaging usually reveals a massive lesion with significant contrast enhancement involving the cerebellum. As mentioned above, medulloblastoma has a high propensity to locally infiltrate leptomeninges, as well as to propagate through the subarachnoid space to involve the ventricles, cerebral convexity, spinal leptomeningeal surfaces. Consequently, it is necessary to study with MRI the entire cranio-spinal axis. [7]. Surgery is entrusted with the task of removing as much of the lesion as possible, in fact post-surgical tumour residues confer a worse prognosis. Pure harbinger of unfavourable prognosis.is the presence of tumour cells in the cerebrospinal fluid or the detection of leptomeningeal metastases at MRI. Surgery alone is usually not curative. The addition of radiotherapy to the cranio-spinal axis, with focus on the primary tumour site, may result. Adding chemotherapy after radiation therapy increases the cure rate. With appropriate treatment, cases of long survival, over 3 years, for medulloblastoma patients, range from 60-80%. [10,22] Diagnosis of atlantoaxial rotatory subluxation is difficult and often delayed. For a correct diagnosis of an AARD, clinical and radiographic evaluation are essential. The possibility of having Dual Energy TC available today allows you to have well-detailed images of the occipital-cervical tract, with limited exposure to ionizing radiation [7,9,14]. MRI will however be irreplaceable for the differential diagnosis for non-traumatic situations [13,15,20,21] We reached the diagnosis that led us to the correct treatment after 4 days from the emergency access of the child. Perhaps the symptoms had been little understood even by the paediatrician for a long period. In our case, the symptomatology made it necessary to do the MRI and it was this examination that led to the diagnosis. In a case like this, delay or miss the diagnosis, could be catastrophic. MRI should be done promptly in every doubtful case [23].
List Abbrevations
AARS Atlanta Axial Rotatory
Subluxation ENT ear Nose Throat
NSAIDs nonsteroidal anti-inflammatory drugs
Declaration
The case report has been presented to the Rizzoli Institute Ethical Committee for approval: they answered there is no need for approval for a case report once the written consent of the patient and family has been recorded.
The written consent to the use and publication of patient data and clinical information for scientific reasons has been signed by the patient father.
Availability of data and materials
They are on the electronic chart and repository of the Rizzoli Ortopedic Institute and the PACS system of the hospital No Competing interests about the facts and materials reported in the paper No funding has been required for the publication.
Authors Contributions
Tiziana Greggi: Writing of the paper
Luca Boriani, Giovanni Ciani, Lucrezia Leggi: Reviewers
Antonio Scarale, Konstantinos Martikos, Francesco Vommaro: Spinal clinical evaluation and treatment. Milva Battaglia: Radiological evaluation
Chiara Ghizzi: Paediatrician of the unit
Mino Zucchelli: Neurosurgical evaluation and treatment
Acknowledgements
We value the great work of our residents, Lucrezia e Giovanni.
References
1. Neal, Kevin M. Mohamed, et al. 2015. Atlantoaxial Rotatory Subluxation in Children, Journal of the American Academy of Orthopaedic Surgeons. 23: 382-392. Ref.: https://pubmed.ncbi.nlm.nih.gov/26001430/
2. Sferopoulos NK. 2018. Atlantoaxial rotatory subluxation in children: A review. J Radiol Med Imaging. 2: 1009.
3. Moore, D. s: www.orthobullets.com/spine/2050/atlantoaxial-rotatory-displacement-aard
4. Louis DN, Perry A, Reifenberger G. et al. 2016. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 131: 803-820. Ref.: https://pubmed.ncbi.nlm.nih.gov/27157931/
5. Greggi T, Scarale A, Maredi E, et al. 2015. The Cervical Trauma in Children: Dificulties in Diagnosis and Treatment Choice. Journal of Spine.
6. Iaccarino C, Francesca O, Piero S, et al. 2019. Grisel's Syndrome: Non-traumatic Atlantoaxial Rotatory Subluxation-Report of Five Cases and Review of the Literature. 125: 279-288. Ref.: https://pubmed.ncbi.nlm.nih.gov/30610334/
7. Hannonen J, Perhomaa M, Salokorpi N, et al. 2019. Interventional magnetic resonance imaging as a diagnostic and therapeutic method in treataing acute pediatric atloaxialrotatory subluxation. Exp Ther. 18: 18-24. Ref.: https://pubmed.ncbi.nlm.nih.gov/31258633/
8. Anene-Maidoh TI, Vega RA, Fautheree GL, et al. 2013. An unusual case of pediatric bow hunter's stroke. Surg Neurol Int. Nov 20l4: 148. Ref.: https://pubmed.ncbi.nlm.nih.gov/24340230/
9. Murray N, Le M, Ebrahimzadeh O. et al. 2017. Imaging the Spine with Dual-Energy CT. Curr Radiol Rep. 5: 44.
10. Kumar LP, Deepa SF, Moinca I, et al. 2015. Medulloblastoma: A common pediatric tumor: Prognostic factors and predictors of outcome. Asian J Neurosurg. 10: 50. Ref.: https://pubmed.ncbi.nlm.nih.gov/25767583/
11. HM, Abruzzo TA, Kabbouche M, et al. 2010. Rotational vertebral artery occlusion in a child with multiple strokes: a case-based update.Greiner Childs Nerv Syst. 26: 1669-1674. Ref.: https://pubmed.ncbi.nlm.nih.gov/20959996/
12. Missori P, Marruzzo D, Peschillo S, et al. 2014. Anene-Maidoh TI, Vega RA, Fautheree GL, Reavey-Cantwell JF. Bow Hunter's syndrome World Neurosurg. 82: 645-648.
13. Goo HW, Goo JM. Dual-Energy CT. 2017. New Horizon in Medical Imaging. Korean J Radiol. 18: 555-569. Ref.: https://pubmed.ncbi.nlm.nih.gov/28670151/
14. Alberto Rufilli MD, Michele Fiore MD, Konstantinos Martikos MD, et al. Does use of pre-operative CT scan in adolescent idiopathic scoliosis improve accuracy in screw placement? Results of a retrospective study"European Spine Journal Springer Journals Editorial Ofice.
15. Nigrovic LE, Rogers AJ, Adelgais KM, et al. 2012. Pediatric Emergency Care Applied Research Network (PECARN) Cervical Spine Study Group. Utility of plain radiographs in detecting traumatic injuries of the cervical spine in children. Pediatr Emerg Care. 28: 426-432.
16. Sobolewski BA, Mittiga MR, Reed JL. 2008. Atlantoaxial rotary subluxation after minor trauma. Pediatr Emerg Care. 24: 852- 856. Ref.: https://pubmed.ncbi.nlm.nih.gov/19092567/
17. Spiegel D, Shrestha S, Sitoula P, et al. 2017. Atlantoaxial rotatory displacement in children. World J Orthop. 8: 836-845. Ref.: https://pubmed.ncbi.nlm.nih.gov/19092567/
18. Fielding JW, Hawkins RJ. 977. Atlanto-axial rotatory fixation. (Fixed rotatory subluxation of the atlanto- axial joint). J Bone Joint Surg Am. 59: 37-44. Ref.: https://pubmed.ncbi.nlm.nih.gov/833172/
19. Murray JB, Ziervogel M. 1990. The value of computed tomography in the diagnosis of atlanto-axial rotatory fixation. Br J Radiol. 63: 894-897. Ref.: https://pubmed.ncbi.nlm.nih.gov/2252986/
20. Scapinelli R. 1994. Three-dimensional computed tomography in infantile atlantoaxial rotatory fixation. J Bone Joint Surg Br. 76: 367-370. Ref.: https://pubmed.ncbi.nlm.nih.gov/8175835/
21. Haque S, Bilal Shafi BB, Kaleem M, 2012. Imaging of torticollis in children. 32: 557-571. Ref.: https://pubmed.ncbi.nlm.nih.gov/22411949/
22. Millard NE, De Braganca KC. 2016. Medulloblastoma [published correction appears in J Child Neurol. 31: 1341-1353. Ref.: https://pubmed.ncbi.nlm.nih.gov/26336203/
23. Louis D, Ohgaki H, Wiestler O, et al. 2007. The 2007 WHO classification of tumours of the central nervous system.Acta Neuropathol. 114: 97-109. Ref.: https://pubmed.ncbi.nlm.nih.gov/17618441/




















