Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/ijcgh.2020.110008Article Views : 38Article Downloads : 15
Asymptomatic free gas post Endoscopic Mucosal Resection (EMR) - Is surgical intervention always necessary?
Shafquat Zaman1*, Hayaka Amada1, Pratik Bhattachayra1, Stephen Stonelake1, Mark Goldstein2 and Misra Budhoo1
1Sandwell and West Birmingham Hospitals NHS Trust, West Bromwich, West Midlands, UK. B71 4HJ
2University Hospitals Birmingham NHS Foundation Trust. Heartlands Hospital, Bordesley Green East, Birmingham, UK. B9 5SS
*Corresponding Author: Mr Shafquat Zaman, Sandwell and West Birmingham Hospitals NHS Trust, West Bromwich, West Midlands, UK. B71 4HJ, Tel: 07944657005; Email: shafquatzaman@nhs.net; shafquatzaman@doctors.org.uk
Article Information
Aritcle Type: Case Report
Citation: Shafquat Zaman, Hayaka Amada, Pratik Bhattachayra, et al. 2020. Asymptomatic free gas post Endoscopic Mucosal Resection (EMR) - Is surgical intervention always necessary?. Int J Clin Gastro Hepato. 2: 19-26.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2020; Shafquat Zaman
Publication history:
Received date: 11 September, 2020Accepted date: 28 September, 2020
Published date: 30 September, 2020
Abstract
Background& Objectives
Endoscopic mucosal resection (EMR) is an efficient, cost-effective and minimally-invasive mode of treatment of colonic polyps. Colonic perforation post EMR is one of the potential complications associated with this procedure. Some patients may present with asymptomatic free gas on imaging and therefore not necessarily require intervention.
Methods
We present a case series of patients undergoing EMR who were found to have intra-abdominal free gas or ‘bowel perforation’ on imaging post procedure. They were all asymptomatic and did not warrant emergency surgical intervention. In addition, we aim to provide a review of the existing literature on ‘bowel perforation’ post EMR and discuss its management.
Results & Conclusion
Through this case series we highlight the importance of assessing patients clinically and not treating the radiological findings alone. Clinicians must be aware of the possibility of patients with asymptomatic free gas post EMR as a direct result of the injectate during the procedure or due to the passage of air or CO2 from the distended colon. As the popularity of this procedure increases, it is crucial that clinicians, surgeons and endoscopists are all aware of its associated complications.
Background & Objectives
Large, complex colonic polyps have traditionally been treated surgically. Colorectal resections performed through open or laparoscopic surgery are not without significant morbidity and mortality. With the development of novel techniques and technological advances, minimally invasive procedures are becoming increasingly widespread to minimise these risks. Endoscopic Mucosal Resection (EMR) has been shown to be safe, efficient, and effective in dealing with large and difficult colonic polyps with substantial cost-savings [1]. Potential complications associated with EMR include the risk of bleeding, bowel perforation, abdominal pain and discomfort, drug reactions and incomplete excision of the target lesion. As EMR is becoming an increasingly effective treatment modality in the management of large sessile polyps, its popularity will continue to increase. It is therefore essential that clinicians and in particular surgeons and endoscopists are aware of this procedure and its associated complications.
In particular, abdominal pain or discomfort experienced by some patients post-procedure often results in a computed tomography (CT) scan being performed as part of the diagnostic process. Clinical features such as localised peritonitis and progression of pain, fever and leucocytosis in the absence of radiographic evidence of colonic perforation has been defined as post-polypectomy syndrome. In order to define the latter point CT is the investigation of choice. Given the incidence of PPS ranges from 0.003-0.1%in general colonoscopy [2] and is higher in EMR and higher still in (up to 9%) in endoscopic submucosal dissection [3], CT scanning is commonplace in the context of the aforementioned symptoms or signs. Knowing what to do when there is radiographic evidence of perforation (0.09% to 3.1% [4-6]) is therefore most relevant for endoscopists. CT scan findings need to be carefully correlated with the patients’ clinical condition before deciding on further management and in particular surgical intervention. We present a case series of three patients who appeared to develop ‘bowel perforation’ on imaging post EMR and discuss their management. We also aim to provide a review of the existing literature on ‘bowel perforation’ post EMR and stress the importance of treating the patient and not the radiological findings.
Methods
Case 1
A 64-year old gentleman who, as part of the national bowel cancer screening programme, underwent elective colonoscopy. The procedure was tolerated well by the patient and the endoscopist noted a lesion 6cm distal to the caecum. This large polyp (40mm) was excised by EMR. The patient’s recovery was unremarkable and he went onto have a scheduled staging CT scan (thorax, abdomen, pelvis) later on the same day. The CT demonstrated incidentally a localised perforation adjacent to the resection site in the ascending colon (Figure 1 - A, B & C). The patient was urgently reviewed on the acute surgical unit by the on-call team. Since he was asymptomatic and clinically well he was reassured and discharged from the hospital.
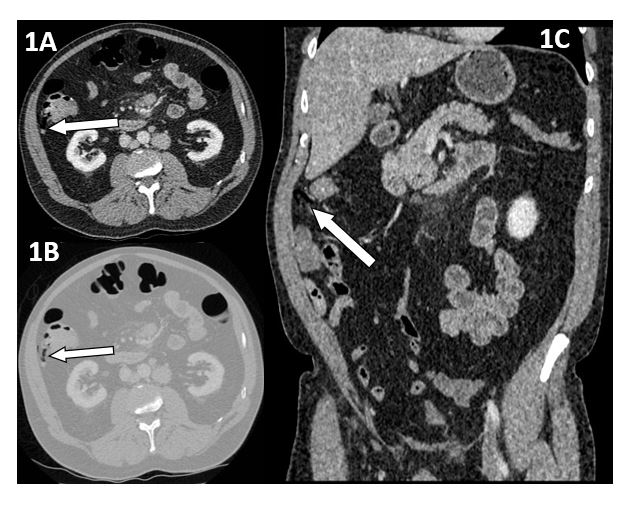
Figure 1 (A,B,C): CT staging for suspected malignancy in the ascending colon demonstrates a linear localised focus of free gas adjacent to the site of EMR demonstrated on axial and coronal views. 1A: Axial view (soft tissue window).1B: Axial view (lung window). Figure 1C: Coronal view.
Case 2
A 71-year old male who again, as part of the national bowel cancer screening programme, underwent elective colonoscopy. A suspicious mass 8cm from the anal verge was seen and biopsied. In addition, EMR of a hepatic flexure polyp (20mm) was performed. Both samples were sent for histological analysis and the patient was informed of the abnormal findings. The patient went on to have a staging CT scan on the same day. This demonstrated significant intra-abdominal free gas, in keeping with a perforated viscus likely secondary to polyp excision (Figure 2-A & B). He was therefore admitted as an emergency and reviewed by the on-call surgical consultant. As he was haemodynamically stable with a soft, non-tender abdomen, he was discharged from hospital after several hours of observation and advised to return in case of clinical deterioration. The patient went on to make a complete and unremarkable recovery.Histology showed a high grade tubular adenoma (hepatic flexure polyp) and a moderately differentiated adenocarcinoma (rectal biopsy). Following discussion at the colorectal MDT he went on to have further definitive elective surgery.
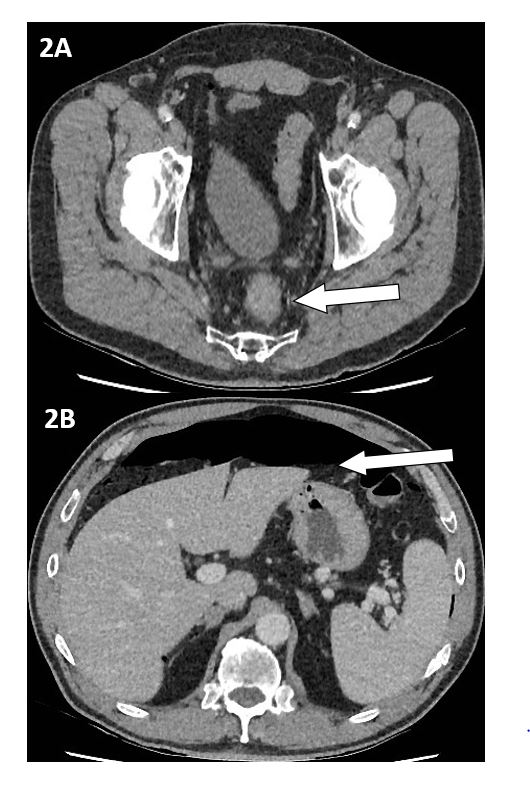
Figure 2 (A,B): CT scan showing irregular circumferential thickening of the rectum(white arrow) in keeping with a rectal malignancy and a large amount of free intra-peritoneal gas (white arrow) several days post EMR in an asymptomatic patient. 2A: Axial view (soft tissue window). 2B: Axial view (soft tissue window), showing large amount of free intra-peritoneal gas.
Case 3
An 84-year old female with a history of abdominal pain, diarrhoea and weight loss underwent a colonoscopy to investigate for malignancy. Prior to the endoscopy, clinical examination revealed a soft abdomen with some mild tenderness on the right side. An impassable colonic stricture, suspicious of malignancy was found and the examination limited to the hepatic flexure. Multiple biopsies (seven) were taken and the area of concern tattooed. The patient had an unremarkable discharge following the Page: 23
www.raftpubs.com
colonoscopy. A planned staging CT scan was performed 6 days later which reported a pneumoperitoneum as a likely sequelae of the recent colonoscopy (Figure 3-A & B). In addition an annular mass in the ascending colon and probable liver metastasis were observed. The patient was reviewed urgently in the surgical outpatient clinic the following day and remained clinically well with no signs or symptoms of peritonitis. An MRI scan was organised to further characterise the liver metastasis and her case discussed at the colorectal multi-disciplinary team (MDT) meeting. Histopathology showed an adenocarcinoma (RAS wild type) and the patient was subsequently referred to oncology for consideration of neo-adjuvant chemotherapy.

Figure 3 (A,B): CT scan showing an annular bowel related mass in the ascending colon suspicious of an annular tumour in addition to a pneumoperitoneum post colonoscopy. 3A: Axial view (soft tissue window), showing large amount of free intra-peritoneal gas. 3B: Coronal view (soft tissue window), showing free intra-peritoneal gas post EMR.
Discussion of Results
Complications of Endoscopic Mucosal Resection
EMR is becoming an increasingly common and viable alternative to surgery in the management of large or complex pre-malignant colorectal lesions [7]. Complication rates are generally low particularly when performed by experienced colonoscopists, with the risk of bowel perforation ranging from 0.09% to 3.1% [4-6,8,9]. Bleeding is the commonest complication with incidence rates ranging from 0.19-24%, and this can either be immediate or delayed. Bowel perforation, as the second commonest complication, may occur as a result of direct endoscope pressure, barotrauma or as a consequence of therapeutic interventions. Non-specific and often self-resolving abdominal pain may be experienced by some patients post-EMR. Symptomatic patients are often investigated by urgent imaging (usually CT) or scans may be performed post-endoscopy in asymptomatic patients for staging purposes. As highlighted in our series of patients, a comprehensive assessment of all patients is required and management decisions should not rely on radiological findings alone. If patients are clinically well and haemodynamically stable, a period of observation prior to hospital discharge may be sufficient. Abdominal CT scans performed soon after EMR may show features consistent with ‘colonic perforation’ including findings of intra-abdominal free gas (localised or more widespread) and fat stranding in the region of polyp removal. However these findings may be secondary to a combination of injectate within the colonic wall and leakage of insufflated air or CO2 following repeated transmural passage of the EMR needle. Clinicians need to be aware of these radiological features of ‘perforation’ post EMR in the absence of an actual EMR-associated perforation [10]. Therefore clinical assessment of the patient is vitally important and can help avert unnecessary laparoscopy or laparotomy and their associated complications.
Review of EMR complications in the literature
Eisenbach et al. found a sessile adenoma (2.5cm) in the caecum of an otherwise healthy 39-year old female with a family history of colon cancer; this was removed via EMR [14]. One day post colonoscopy, their patient presented with generalised abdominal pain. Plain radiographs showed a pneumoperitoneum resulting in the patient undergoing an emergency ileocaecal resection. Apart from a ceacal wall haematoma, no obvious perforation or peritonitis was demonstrated intra-operatively. The histology of the resected specimen showed a defect at the polyp resection site penetrating down to the muscularispropria, with granulocyte infiltration and caecal wall pneumatosis. This case report demonstrated no macroscopic or histological evidence of a transmural breach of the colonic wall. It suggested that the presence of the pneumoperitoneum may be in keeping with translocation of insufflated air through a thinned colonic wall. Therefore this patient could have instead been kept under close observation and their major surgery prevented. The sensitivity of CT scanning in diagnosing extramural versus intramural in thinned out bowel also must be considered here. Stephenson et al. reported on a 51-year old Caucasian female who underwent EMR of a 30mm sessile mid-descending colonic polyp. She developed severe left iliac fossa pain 2hours post-procedure without any systemic upset or compromise. Urgent CT scan of the abdomen showed intra-mural gas at the site of polyp excision with adjacent fat stranding but no free gas. The patient was managed conservatively and discharged the following day [15]. Post-polypectomy electrocoagulation syndrome is a recognised complication [16].
This occurs due to diathermy current extending past the mucosa into the deeper bowel layers causing a transmural burn without perforation. Injecting or lifting polyps helps to reduce this phenomenon. As a result of serosal irritation, patients can present usually several hours to days post procedure with severe abdominal pain including signs of localised peritonism. It is important that radiologists too are aware of ‘normal’ CT appearances post EMR so that these are reported correctly. Colonic wall transmural thickening in the resection area, oedema and intramural gas may all be seen. Tribonias (2018) reported on a case of a 76-year old male, with previous right hemicolectomy due to colorectal cancer who underwent EMR for 35mm distal sigmoid polyp. He experienced severe left sided abdominal pain post procedure. Urgent CT showed diffuse bowel wall thickening and oedema, intramural gas and a single extraluminal gas bubble with adjacent fat stranding. The patient was managed conservatively with pain settling completely after several hours [17]. Lim et al. (2017) performed a retrospective observational study (n=564) over a 9-year period to assess their EMR service [18]. They identified a single case of immediate perforation post EMR of an 80mm caecal villous adenoma which was managed endoscopically with endoclips. In addition, there were 2 patients in their cohort requiring endoscopic treatment for delayed bleeding. 3.3% had post-polypectomy pain syndrome but no re-admissions were noted for delayed perforation requiring surgery.These cases, alongside those reported by our institution, demonstrate the variety of post-EMR complications, many of which can be managed conservatively. These include transmural diathermy burns, colonic wall haematoma, delayed bleeding, and aspects of post polypectomy pain syndrome. Awareness of these and other complications is crucial for clinicians - endoscopists, radiologists, and surgeons, to have a balanced set of differentials.
Conclusion
In the absence of any endoscopic suspicion for bowel perforation, CT scan findings of intramural and extraluminal gas could be due to leakage of air from the injectate during attempts with the EMR needle to lift the polyp off the mucosa. Alternatively, the tiny hole created by the EMR needle may allow passage of air or CO2 from the distended colon giving a clinical appearance of ‘true’ bowel perforation. EMR is a safe and effective minimally invasive therapeutic intervention. In all cases of abdominal pain post EMR, prompt surgical review is essential. A period of observation may be necessary prior to hospital discharge. Good communication between the endoscopist, surgical team and radiologists is critical to prevent unnecessary interventions, particularly surgery and its associated risks.
References
1. Bourke M. 2011. Endoscopic mucosal resection in the colon: A practical guide. Tech Gastrointest Endosc. 13: 35-49.
2. Ko CW, Dominitz JA. 2010. Complications of colonoscopy: magnitude and management. GastrointestEndoscClin N Am. 20: 659-671. Ref.: https://pubmed.ncbi.nlm.nih.gov/20889070/
3. Hirasawa K, Sato C, Makazu M, et al. 2015. Coagulation syndrome: Delayed perforation after colorectal endoscopic treatments. World J GastrointestEndosc. 7: 1055-1056.
4. De Ceglie A, Hassan C, Mangiavillano B, et al. 2016. Endoscopic mucosal resection and endoscopic submucosal dissection for colorectal lesions: A systematic review. Crit Rev OncolHematol. 104: 138-155. Ref.: https://pubmed.ncbi.nlm.nih.gov/27370173/
5. Ma MX, Bourke MJ. 2016. Complications of endoscopic polypectomy, endoscopic mucosal resection and endoscopic submucosal dissection in the colon. Best Pract Res ClinGastroenterol. 30: 749767. Ref.: https://pubmed.ncbi.nlm.nih.gov/27931634/
6. Lee EJ, Lee JB, Lee SH, et al. 2012. Endoscopic treatment of large colorectal tumors: comparison of endoscopic mucosal resection, endoscopic mucosal resection-precutting, and endoscopic submucosal dissection. SurgEndosc. 26: 2220-2230.
7. Swan MP, Bourke MJ, Alexander S et al. 2009. Large refractory colonic polyps: is it time to change our practice? A prospective study of the clinical and economic impact of a tertiary referral colonic mucosal resection and polypectomy service (with videos). Gastrointest Endosc. 70: 1128-36.
8. Moss A, Bourke MJ, Williams SJ et al. 2011. Endoscopic mucosal resection outcomes and prediction of submucosal cancer from advanced colonic mucosal neoplasia. Gastroenterology.; 140: 1909-1918.
9. Heldwein W, Dollhopf M, Rosch T et al. 2005. The Munich Polypectomy Study (MUPS): prospective analysis of complications and risk factors in 4000 colonic snare polypectomies. Endoscopy. 37: 1116-1122. Ref.: https://pubmed.ncbi.nlm.nih.gov/16281142/
10. Heerasing N. 2013. Abdominal pain post endoscopic mucosal resection: Treat the patient not the CT scan. World J Gastrointest Endosc. 5: 455-456. Ref.: https://pubmed.ncbi.nlm.nih.gov/24044046/
11. de’Angelis N, DiSaverio S, Chiara O et al. 2018. 2017 WSES guidelines for the management of iatrogenic colonoscopy perforation. World J. Emerg. Surg. 13: 5. Ref.: https://pubmed.ncbi.nlm.nih.gov/29416554/
12. Wang J, Zhang XH, Ge J et al. 2014. Endoscopic submucosal dissection vs endoscopic mucosal resection for colorectal tumors: A meta-analysis. World J Gastroenterol. 20: 8282-8287. Ref.: https://pubmed.ncbi.nlm.nih.gov/25009404/
13. Sethi A, Song LM. 2015. Adverse events related to colonic endoscopic mucosal resection and polypectomy. GastrointestEndoscClin N Am. 25: 55-69. Ref.: https://pubmed.ncbi.nlm.nih.gov/25442958/
14. Eisenbach C, Bläker H, Stremmel W et al. 2008. Pneumoperitoneum following endoscopic mucosal resection without perforation of the colon. Endoscopy. 2: 64-65.
15. Stephenson JA, Crookdake J, Jepson S et al. 2013. Imaging findings post colorectal endoscopic mucosal resection. J Radiol Case Rep. 7: 27-32. Ref.: https://pubmed.ncbi.nlm.nih.gov/24421955/
16. Benson BC, Myers JJ, Laczek JT. 2013. Postpolypectomy Electrocoagulation Syndrome: A Mimicker of Colonic Perforation. Case Rep Emerg Med. 687931. Ref.: https://pubmed.ncbi.nlm.nih.gov/23956889/
17. Tribonias G, Daferera N, Manola M-E et al. 2018. How familiar are we with decision-making concerning the treatment of perforation after endoscopic mucosal resection (EMR) in the colon? A case report. Endosc Int Open. 6: 308-312. Ref.: https://pubmed.ncbi.nlm.nih.gov/29507871/
18. Nyuk Fung Lim D, Robinson R, Wurm P et al. 2017. Outcome of An Endoscopic Mucosal Resection Service for Large Sessile Colonic Polyps (≥ 20 mm) over A 9-Year Period: A Single Centre Experience and Analysis of Change over Time in A University Teaching Hospital. J Gastroenterol Hepatol Res. 6: 2318-2323.




















