Indexing & Abstracting
Full Text
Research ArticleDOI Number : 10.36811/ijcgh.2021.110010Article Views : 50Article Downloads : 42
Reduction in ERCP volume for Acute Cholangitis and other Indications during COVID-19 Pandemic
Swathi Paleti MD, Zain A. Sobani MD and Tarun Rustagi MD*
Division of Gastroenterology and Hepatology, Department of Internal, Medicine, University of New Mexico, NM, USA
*Corresponding Author: Tarun Rustagi MD, Division of Gastroenterology and Hepatology, Department of Internal Medicine, University of New Mexico, MSC10 5550, 1 University of New Mexico, Albuquerque NM 87131, Tel: +1-860-221-4034; Fax: +1- 505-272-9751; Email: tarunrustagi06@gmail.com
Article Information
Aritcle Type: Research Article
Citation: Swathi Paleti, Zain A. Sobani, Tarun Rustagi. 2021. Reduction in ERCP volume for Acute Cholangitis and other Indications during COVID-19 Pandemic. Int J Clin Gastro Hepato. 3: 01-04.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2021; Swathi Paleti
Publication history:
Received date: 21 December, 2020Accepted date: 08 January, 2021
Published date: 11 January, 2021
Abstract
Introduction: The COVID-19 pandemic continues to significantly impact healthcare with Joint Gastrointestinal Societies recommending rescheduling elective and non-urgent endoscopic procedures. The aim of our study was to evaluate the trend of acute cholangitis requiring emergent ERCP and overall ERCP practice in the setting of the COVID 19 pandemic.
Methods: A retrospective review of all ERCPs performed at our institution was performed during the study period (3/16/2020 to 4/15/2020) along with the preceding 2 months (1/1/2020 to 2/29/2020) and similar time period from the last 2 years (3/16/2019 to 4/15/2019 and 3/16/2018 to 4/15/2018) for comparison to account for any seasonal variation.
Results: A reduction was noted in absolute number and proportion of ERCPs performed for acute cholangitis during the study period compared to preceding months (2 [6.45%] vs. average 10.5 [15.05%] cases/month; 81% reduction). We also found reduction in overall number of both inpatient and outpatient ERCPs during the study period (31 ERCPs/month to average 70 ERCPs/month; 55% reduction in ERCP volume).
Conclusions: There was a reduction in the overall ERCP volume and number of ERCPs performed for acute cholangitis during the COVID-19 pandemic. Further larger studies are needed to validate this data and investigate its causes.
Keywords: ERCP; COVID-19; SARS-2-Cov; Pandemic; Acute cholangitis; Trend; Biliary
Introduction
The current pandemic of COVID-19 has significantly altered every aspect of life, especially the healthcare system. With evidence suggesting the potential for viral transmission through droplets and perhaps fecal shedding, [1,2] countries and regions have implemented different strategies to mitigate the spread of the virus. These strategies have a common underlying theme of social distancing, avoiding unnecessary travel, and minimizing social gatherings. In order to further mitigate the spread and conserve precious personal protective equipment, the Surgeon General of the United States recommended deferring elective medical procedures on March 14th, 2020. Following this, the Joint Gastrointestinal Societies- American Gastroenterological Association (AGA), American College of Gastroenterology (ACG), American Association for the Study of Liver Diseases (AASLD) and American Society for Gastrointestinal Endoscopy (ASGE) strongly recommended rescheduling elective and non-urgent endoscopic procedures. Based on these recommendations we postponed all non-urgent procedures in at our institution with effect from March 16th, 2020. In addition to discontinuing non-urgent procedures, being the only tertiary high-volume (>750 ERCPs/year) referral academic center in the State of New Mexico we expected to see a surge of referrals from other medical centers. We started a contingency planning for an increase in the number of referrals for urgent endoscopic retrograde cholangiopancreatography (ERCP) in the setting of acute cholangitis. This was based on the assumption that the baseline incidence of acute cholangitis would not be altered by the measures to prevent viral transmission. The aim of this study was to evaluate the trend of acute cholangitis requiring emergent ERCP and overall ERCP practice in the setting of the COVID 19 pandemic.
Methods
We conducted a retrospective review of all ERCPs performed at our institution during the study period (3/16/2020 to 4/15/2020). In addition, we collected similar data from the preceding 2 months (1/1/2020 to 2/29/2020) and similar time period from the last 2 years (3/16/2019 to 4/15/2019 and 3/16/2018 to 4/15/2018) for comparison to account for any seasonal variation. Demographic, endoscopic, and clinical data was abstracted and analyzed. Descriptive analysis was performed by calculating means and standard deviations for continuous variables and proportions for categorical ones.
Results
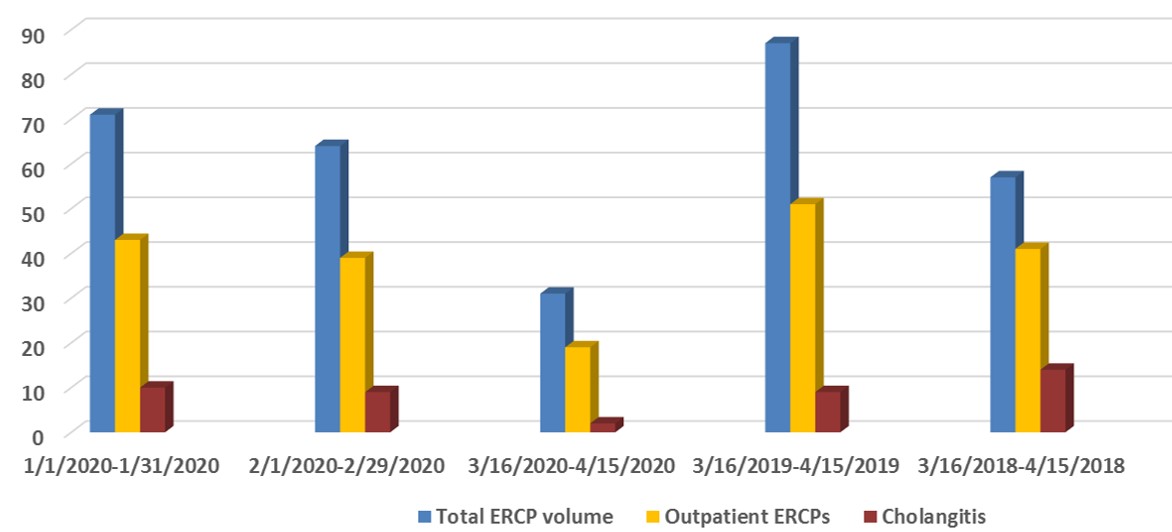
We found a reduction in the absolute number and proportion of ERCPs performed for acute cholangitis during the study period compared to preceding months (2 [6.45%] vs. average 10.5 [15.05%] cases/month; 81% reduction) [Table 1, Figure 1]. The overall number of both inpatient and outpatient ERCPs decreased during the study period (31 ERCPs/month to average 70 ERCPs/month; 55% reduction in ERCP volume) with reduction in ERCPs performed for pancreatic and non-cholangitis biliary indications [Table 1, Figure 1].
|
Table 1. ERCP volume and indications during the study period compared to prior months. |
|||||
|
|
1/1/2020-1/31/2020 |
2/1/2020-2/29/20202 |
3/16/2020-4/15/2020 |
3/16/2019-4/15/2019 |
3/16/2018-4/15/2018 |
|
Age |
56.5±17.7 |
55.3±17.6 |
54.4±19.5 |
57±19.2 |
60.3±18.4 |
|
Gender (% female) |
59.2 |
54.7 |
35.5 |
57.5 |
38.6 |
|
Total ERCP volume |
71 |
64 |
31 |
87 |
57 |
|
Outpatient ERCP (%) |
60.6 |
60.9 |
61.3 |
58.6 |
71.9 |
|
Indications: · Acute cholangitis · Non-cholangitis biliary · Pancreatic |
10 46 15 |
9 44 11 |
2 27 2 |
9 67 11 |
14 37 6 |
Discussion
When planning and preparing for the COVID 19 pandemic we expected a rise in the use of healthcare resources. The expectation was to have the same baseline prevalence of emergent conditions including exacerbations of chronic disease, infections, gastrointestinal emergencies, cerebrovascular and coronary events with the addition of the patients presenting with COVID 19. Further being the only tertiary referral center in the state we expected an increase in the number of referrals for these conditions. However, an interesting trend seems to have emerged - we have seen a decrease in healthcare utilization for other indications. We particularly looked at acute cholangitis as it is one of the few urgent diagnoses under our umbrella requiring urgent endoscopic intervention. The fever, abdominal pain, and jaundice are not symptoms a patient would easily ignore. Further acute cholangitis is not a diagnosis that can be temporized with medical management and deferring definitive therapy to a later date can be detrimental. Source control with emergent ERCP within 48 hours of presentation has been associated with a reduction in mortality, organ failure and length of stay [3]. In our study, we found a 55% reduction in the number of ERCPs performed, which was certainly expected given the cancelation of non-emergent procedures. An unexpected reduction in the number of patients requiring ERCP for acute cholangitis was also noted. On average we perform 10.5 ERCPs for acute cholangitis each month which was reduced by 81% to 2 during the study period. This reduction in acute cholangitis is intriguing as cancellation of elective and semi-elective procedures such as asymptomatic choledocholithiasis and routine biliary stent changes should have potentially resulted in an increase in number of cases of biliary obstruction. Further COVID-19 has been associated with elevation of liver enzymes with concurrent fever which would also have caused an increase in the number of patients with suspected cholangitis [4,5]. Similar trends have also been seen for other emergent diagnosis such as myocardial infarctions. Garcia et al expected to find an increase in the number of myocardial infarctions resulting in increased cardiac catheterization laboratory activations given heightened environmental and psychosocial stressors; however, they conversely found a 38% reduction [6].
One possible hypothesis is that the decrease in acute cholangitis cases could be attributed to avoidance of medical care due to social distancing or due to fear of exposure to COVID-19 in the hospital. Though this is questionable as the symptoms of acute cholangitis are hard to ignore in most cases. Another plausible explanation includes the use of antibiotic therapy alone without referral for ERCP due to COVID-19 scenario. It is unclear what is leading to the reduction in the presentation of these emergent diagnosis. As the pandemic evolves, we plan to continue to follow this early signal and investigate its causes. It is particularly crucial to understand if patient-based anxiety is decreasing presentation of acute cholangitis patients to the healthcare system.
References
1. Xiao F, Tang M, Tang X, et al. 2020. Evidence for Gastrointestinal Infection of SARS-CoV-2. Gastroenterology, 2020. Ref.: https://pubmed.ncbi.nlm.nih.gov/32142773/
2. Gu JB, Han J. Wang. 2020. COVID-19: Gastrointestinal Manifestations and Potential Fecal-Oral Transmission. Gastroenterology. Ref.: https://pubmed.ncbi.nlm.nih.gov/32142785/
3. Iqbal U, Khara H, Hu Y, et al. 2020. Emergent versus urgent ERCP in acute cholangitis: a systematic review and meta-analysis. Gastrointest Endosc. 91: 753-760. Ref.: https://pubmed.ncbi.nlm.nih.gov/31628955/
4. Cai Q, Chen J. 2020. Characteristics of Liver Tests in COVID-19 Patients. J Hepatol. Ref.: https://pubmed.ncbi.nlm.nih.gov/32387074/
5. Sun C, Zhang XB, Dai y, et al. 2020. Clinical analysis of 150 cases of 2019 novel coronavirus infection in Nanyang City, Henan Province. Zhonghua Jie He He Hu Xi Za Zhi. 3: 42. Ref.: https://pubmed.ncbi.nlm.nih.gov/32295322/
6. Garcia S, Albaghdadi M, Meraj P, et al. 2020. Reduction in ST-Segment Elevation Cardiac Catheterization Laboratory Activations in the United States during COVID-19 Pandemic. J Am Coll Cardiol. Ref.: https://pubmed.ncbi.nlm.nih.gov/32283124/




















