Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/jcri.2019.110002Article Views : 2466Article Downloads : 19
Conservative management of post-traumatic sialocele of the parotid gland: A case report
Ahmed A El-Degwi1* and Mohamed Ashraf Elkahwagi2
1Professor of ORL, HNS Mansoura University, Egypt
2Assistant lecturer, MD of ORL, HNS Mansoura University, Egypt
*Corresponding author: Ahmed Ali El-degwi, Professor of ORL, HNS Mansoura University Egypt, Email: adegwi57@yahoo.com
Article Information
Aritcle Type: Case Report
Citation: Eldegwi AA, Elkahwagi MA. 2019. Conservative management of post-traumatic sialocele of the parotid gland: A case report. J Case Rept Img. 1: 09-14.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2019; Eldegwi AA
Publication history:
Received date: 22 December, 2018Accepted date: 18 January, 2019
Published date: 19 January, 2019
Abstract:
Introduction: posttraumatic cystic swelling in the parotid region has a complex diagnosis and requires careful management. Posttraumatic siaolcele has two main line of management: one that preserves the gland function and other that depresses the gland function.
Methods: a case report of a posttraumatic sialocele managed by conservative measure including sterile aspiration and bandage. Ultrasonography, Computed Tomography and sialography were the main investigations that aided the diagnosis. The case was followed up for 6 months
Results: aspiration of the fluid contents revealed complete evactuation of the cyst. Complete resolution was achieved by 3 weeks after aspiration.
Conclusion: posttraumatic parotid sialocele is uncommon cause of parotid swelling. Careful mangemnt is mandatory and gland function preservation is the optimum line of management.
Keywords: Posttraumatic; Sialocele; Parotid
Introduction
A post-traumatic parotid sialocele is an acquired lesion that arises from extravasation of saliva into the glandular or periglandular tissues secondary to disruption of the parotid duct or parenchyma [1,2]. Traumatic causes include sharp penetrating wounds in the oral cavity or in the face and blunt trauma, such as zygomatic and mandible fractures [3,4]. Sialocele typically presents 8-14 days after the trauma [5].
Mucoceles are round and well-defined lesions that contain mucin. When they occur in major salivary gland, they are called sialocele. Mucoceles are of two types: extravasation and retention. Mucous extravasation phenomenon is when mucous is extruded into the connective tissue and is surrounded by granulation tissue. Mucous retention phenomenon is used to describe a cyst with retained mucin lined with ductal epithelium [6].
Differential diagnosis of sialocele includes retention cyst, sialodochitis, branchial cleft cyst and lympho-epithelial cyst. Sialocele is not a common condition so the thinking about it is not straight forward. However, given a history of facial trauma or surgery, the diagnosis of traumatic sialocele can be made. In equivocal cases, an elevated amylase level in aspirate or imaging can help in establishing the diagnosis [6].
Management of posttraumatic sialocele shows great controversies. Many treatment modalities have been mentioned in the literature. They basically consist of two main lines; one that preserve the gland function and other that depress it; a conservative or a surgical approach [5,7-9]. A conservative modality is that one that preserve the gland function and is based on regular aspiration of the content, compression dressing and administration of an antisialogogue [5]. Drugs act by blocking acethylcoline release, thereby inhibiting neurotransmission at the secretomotor parasympathetic autonomic nerve ending responsible for salivation. When conservative management fails, or when the overlying skin become so thin that there is imminent risk of rupture, surgical treatment is indicated. Surgery may be performed by repair or reconstruction of the duct, creation of a controlled internal fistula, superficial or total parotidectomy, parasympathetic denervation and ductal ligation [10].
This paper reports a case of a posttraumatic parotid sialocele in an adult patient and how it was managed successfully by preservative approach instead of depressive one for the function of the gland.
Case Report
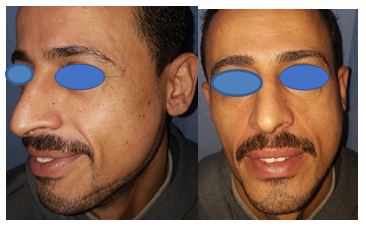
A thity five years old male patient presented with a 3-week history of swelling over his left cheek just inferior to the ear. He was referred after healing of large stab wound to the face; the wound started from the root of the helix of the auricle to the chin at the level of the canine tooth (Figure 1a). He denied any episodes of fever lately in his medical history. There was no associated pain or alteration of facial function as well as no motor or sensory deficits were observed.
The swelling measured about 3 cm in length and 2.5 cm in width. On palpation an ill-defined and resilient mass was noticed (Figure 1b). This mass was evident extra orally with a considerable bulging of the skin in the left parotid region. The lesion was normal and no lymphadenopathy was detected. On intraoral examination, oral mucosa and teeth were healthy. The parotid duct in the affected side was normal and salivary flow had normal physical aspects without debris or purulent discharge. Ultrasonography revealed a hypoechoic ovoid well defined image suggesting a cyst that was well defined lesion measuring 3.5 cm length and 2.5 cm seen on the anterior margin of the parotid gland inseparable from the parotid gland and masseter muscle. No abnormal enhancement after contrast administration. There was a possible defect in the anterior aspect of the parotid duct on sonography (Figure 2). Computed axial and coronal tomography confirmed the ultrasonography findings with expansion to the subcutaneous space at the angle of the mandible (Figure 3a,b).
Figure 1a: The stab wound, Figure 1b: Swelling in parotid region.

Figure 2: The ultrasonography showed the cyst.

Figure 3a: Axial CT showing intraparotid cyst, Figure 3b: coronal CT showing intraparotid cyst.

The panoramic radiograph showed that the teeth and bones are preserved without any evidence of abnormalities. Sialography of the left parotid was performed using Lipiodol as a substance of contrast. A partial filling of the gland was enough to show cavitary sialectasia, and the contrast was retained in the gland for 24 hours (Figure 4).
Figure 4: Retention of contrast after 24 hours in sialography.

Procedure
Decision making in such case was quiet difficult. Conservative measure versus superficial parotidectomy were the main advocated line of treatment for the recent history of trauma and the cystic consistency of the swelling we decided to do aspiration followed by bandage as a preservation way for the parotid gland function.
A percutaneous needle aspiration of the swelling was performed 2 weeks after the sialography. It yielded 14 mL of a clear faint yellowish viscous fluid. The material was submitted to microbiological analysis and showed numerous polymorphonuclear leukocytes. The fluid did not show any bacterial growth and presented high amylase levels (6,000 units/L). The aspiration procedure was sufficient to empty the cavity. A firm bandage was put with double dressing over the site of the swelling; the color of the skin was checked to ensure that no vascular compression before discharge of the patient. The patient was discharged with the bandage and advised to follow up twice a week for three weeks. Three days after the percutaneous aspiration no swelling was observed. The overlying skin did not show any change of color or erythema on the surface of the mass, no signs of infection, and the patient did not report a signficant pain (Figure 5). At the 21-day follow-up visit, complete recovery was noticed, and the residual swelling had totally disappeared. Six months follow up revealed complete resolution and non-recurrence of the condition.
Discussion
There are few reported cases of the formation of a sialocele or salivary fistula secondary to blunt trauma to the parotid gland, a search of the literature reveals few cases [7,11]. Sialocele is most commonly seen in parotid gland and rarely in submandibular and sublingual glands [12].
An injury classification system has been advocated by Van Sickels. This system divides the parotid injuries into three regions: 1. Posterior to the masseter or intraglandular (site A), 2. Overlying the masseter (site B), and 3. Anterior to the masseter (site C) [10].
Figure 5: Three weeks after percutaneous aspiration.
Causes of sialocele formation include: Trauma (sharp penetrating wounds, road traffic accidents and blunt trauma), Infections (infected tooth, tuberculosis and syphilis), Maxillo facial surgeries like Temporomandibular joint surgery and parotidectomy [4,13].
The diagnosis is complex and involves a combination of thorough history and clinical assessment of the patient, fine needle aspiration and image analysis [14]. Fine needle aspiration is a standard technique which permits sampling and the fluid may be submitted to further investigation. Imaging studies include sialography, ultrasonography, computed tomography (CT) and magnetic resonance imaging [10].
The sialography is a technique that visualizes the extravasation of the fluid in the gland substance but can have rare complication. CT may show details of the area, such as a single or multiloculated cystic lesion with regular margins and lower density of the surrounding tissues [10].
The management of a patient with a swelling in the parotid region requires careful clinical evaluation. Fine-needle aspiration or biopsy is necessary for a definite diagnosis. Sialography, computed tomography and ultrasonographic scans may be very helpful. Sialography of the parotid gland was mandatory in revealing the cyst in our case and is also useful to distend the duct when it is involved
An important matter for the diagnosis and treatment was fine-needle aspiration, which provided the fluid for analysis of the serum amylase. Parotid secretion has a high amylase content that is usually around 10,000 units/L. In the present case, the amylase content was 6,000units/L, and that confirmed the diagnosis of parotid saliva extravasation.
Sterile aspiration followed by pressure bandage was effective manner to preserve the gland function and had excellent outcome. The authors advocate this line of management to be the first line in cases of posttraumatic sialocele and this is similar to other studies [1,8,14] but differs from the depressive lines of management as parotidectomy that was advocated in other studies [7,12].
Relative rarity of this condition is a limitation, so the description is usually in the form of case reports. Consensus on management algorithm for this problem should be advocated in future studies.
Conclusion
Posttraumatic parotid sialocele is a rare entity and should be diagnosed carefully. Conservative treatment by aspiration and pressure bandage represents the main line of treatment as it preserves the gland function and has the best outcome if well-done in selected case with confined cysts without infection.
References
- Ns M, Singh M, Roopak B, et al. 2016. Conservative management of parotid fistula and sialocele. 4: 61-64.[Ref.]
- Rathi A, Sagtani A, Sybil D, et al. 2010. Case Note Parotid sialocele: A case report. 11: 154-156.[Ref.]
- Canosa A, Cohen MA, Dent M, et al. 1999. Post-Traumatic Report Parotid Sialocele?: of Two Cases. 742-745.[Ref.]
- Hwang J. 2018. Treatment of intractable parotid sialocele occurred after open reduction-fixation of mandibular subcondylar fracture. 19: 157-161.[Ref.]
- Singh MA, Rangaswamy S. 2011. Parotid Sialocele and Fistulae: Current Treatment Options.[Ref.]
- Kulkarni AM, Rajgopal D, Kulkarni BM, et al. 2014. Non traumatic parotid sialocele: A case report. 2: 53-55. [Ref.]
- Falk J, Borgwardt R, Macleod S, et al. 2017. Posttraumatic Parotid Sialocele Complicating a Mandibular Fracture: A Case Report. 314-317.[Ref.]
- Conservative approach for Parotid Sialocele: A Review. 2015; 2: 48-51. [Ref.]
- Hofer TD, Alucema SD, Pozo JA. 2015. Delayed Treatment of Parotid Sialocele: A Functional Approach and Review. J Oral Maxillofac Surg [Internet]. 73: 284-290.[Ref.]
- Bitra S, Kashinath MS, Zuhaib M, et al. 2016. Parotid Sialocele: A Literature Review. 1: 16-18. [Ref.]
- Sialocele of Parotid Duct: Report of Case with Review of Literature. 10: 4-5.[Ref.]
- Bakshi J. 2018. Sialocele-A Rare Entity Following Submandibular Gland Excision. 4-6.[Ref.]
- Joshi P, Seth N. 2014. Case Report: An Unusual Case of Preauricular Swelling, Parotid Sialocele. 405-408.[Ref.]
- Araujo MR De, Centurion BS, Albuquerque DF De. 2010. Management of a parotid sialocelein a young patient: case report and literature review. 18: 432-436.[Ref.]




















