Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/jcri.2019.110007Article Views : 36Article Downloads : 41
Unexpected diagnosis resulting from presentation with Chronic Obstructive Pulmonary Disease (COPD) exacerbation
C Farrell*, M Goggins and B Casserly
Respiratory Department, University Hospital Limerick, Limerick, Ireland
*Corresponding author: Dr Ciaran Farrell, Respiratory Department, University Hospital Limerick, Limerick, Ireland, Email: ciarandfarrell@gmail.com
Article Information
Aritcle Type: Case Report
Citation: C Farrell, M Goggins, B Casserly. 2019. Unexpected diagnosis resulting from presentation with Chronic Obstructive Pulmonary Disease (COPD) exacerbation. J Case Rept Img. 1: 43-47.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2019; C Farrell
Publication history:
Received date: 06 June, 2019Accepted date: 13 June, 2019
Published date: 14 June, 2019
A bronchocele (bronchial mucocele) is a cystic formation caused by impacted mucoid secretion within the bronchial tree. Non-obstructive causes include bronchiectasis, cystic fibrosis, and asthma while obstructive causes include foreign bodies, benign strictures, congenital bronchial atresia, and in rare cases neoplasms. We describe the case of a 79-year-old male presented with increasing shortness of breath and pleuritic chest pain. He was treated for an infective exacerbation of chronic obstructive pulmonary disease (COPD). He was a current smoker with greater than a 40-year pack history. D-dimers were elevated at 1.49 and he underwent a computed tomography pulmonary angiogram that showed lobulated mass in the right lower lobe suggestive of a bronchocele. The patient underwent a bronchoscopy that demonstrated findings consistent carcinoid tumor. Transbronchial biopsies surprisingly revealed moderately differentiated squamous cell carcinoma. In rare cases, neoplasms have been associated with bronchoceles emphasising the importance of bronchoscopy (for direct visualisation) and biopsy in the workup.
Keywords: Bronchocele; Bronchoscopy; Carcinoid tumour; Squamous cell carcinoma
Introduction
A bronchocele (bronchial mucocele) is a cystic formation caused by impacted mucoid secretion within the bronchial tree. Non-obstructive causes include bronchiectasis, cystic fibrosis, and asthma while obstructive causes include foreign bodies, benign strictures, congenital bronchial atresia, and in rare cases neoplasms. Computed tomography may demonstrate a fluid-filled density with the classic finding of finger-in-glove sign. While CT may also intimate the disease process underlying the bronchocele, bronchoscopy with biopsy is required to confirm the diagnosis.
Lung neuroendocrine tumors (bronchial carcinoid) account for 1–2% of all lung malignancies in adults and on average 20–30% of all neuroendocrine tumors. Typical carcinoid tumours which are the most common subtype, representing 85–90% are predominantly benign., Atypical carcinoid tumours account for 10–15% and may exhibit malignant features. Computed tomography may demonstrate well defined soft-tissue attenuation, usually in a central airway in which the proximal airway may be slightly widened. Seventy-five percent of lung neuroendocrine tumors are centrally located and amenable to biopsy via bronchoscopy. Their typical appearance is a pink-to-red vascular mass with intact overlying bronchial epithelium.
Squamous cell carcinoma is the second most common lung malignancy, accounting for 21.5% of the total [1]. Computed tomography may demonstrate 1) mediastinal infiltration of tumor, 2) mediastinal lymphadenopathy (lymph nodes >1 cm in short-axis diameter on the transverse CT image), 3) hilar lymphadenopathy/central tumor (proximal one-third of hemithorax) or 4) peripheral tumor. Bronchoscopy may demonstrate a necrotic mass, hemorrhage, or irregular mucosa.
Case Presentation
We describe the case of a 79-year-old male admitted to our center with an exacerbation of chronic obstructive pulmonary disease (COPD). Other background history includes prostate cancer, diabetes mellitus type II, hypertension, and chronic obstructive pulmonary disease. He was a current smoker with greater than a 40-year pack history.
During his initial admission he presented with pleuritic chest pain and an elevated D-dimer at 1.49 microgram/millilitre (0.01-0.50). He underwent a chest x-ray and CT pulmonary angiogram that showed a prominent mucous plug of the right lower lobe, bilateral emphysematous changes, a calcified right perifissural granuloma, but no evidence of pulmonary embolus (Figure 1a and 1b). Arterial blood gas on room air showed a pH of 7.56, pCO2 3.55 kPa, PO2 14 kPa, and HCO3- of 26.5 mmol/L. Laboratory analysis revealed a c-reactive protein (CRP) of 13 milligram/decilitre (mg/dL). After two days in hospital, he was discharged on a course of oral Co-Amoxiclav.

Figure 1a: Admission chest x-ray.

Figure 1b: Initial CTPA.
Five weeks later he represented with an infective exacerbation of COPD. There was a three-week history of dyspnea on exertion, expiratory wheeze, pleuritic chest pain, and a productive cough. The patient denied any symptoms of hemoptysis or weight loss. Laboratory analysis revealed a CRP of 167 mg/dL, Na of 125 mmol/L white cell count 9.1 109/litre. Venous blood gas in room air showed a pH of 7.323, pCO2 of 6.67 kilopascals, and HCO3- of 22.8 millimol/litre. Chest x-ray showed evidence of persistent rounded airspace opacities in the right lower lobe with interval onset triangular-shaped airspace opacification in the right lower lobe. An outpatient bronchoscopy and repeat CT thorax was organised. He was commenced on intravenous hydrocortisone and anti-microbials. In total, he completed a seven-day course of Piperacillin-tazobactam and nine days of Clarithromycin before being discharged on a five-day course of Augmentin and a four-day course of oral prednisolone.
Seven weeks after his initial presentation he was readmitted with another infective exacerbation of COPD and was commenced on intravenous hydrocortisone and Co-Amoxiclav. Chest x-ray during the admission showed that the right lower lobe lesion appeared to have increased in both size and density. Laboratory analysis revealed a CRP of 21 mg/dL. He was discharged on a five-day course of oral Co-Amoxiclav and a tapering dose of Prednisolone. Eleven weeks after the initial presentation a repeat CT thorax and bronchoscopy was performed. CT Thorax with contrast showed significant background emphysema and a right basal lobulated mass just under 4 cm in diameter with an intraluminal component; an interval increase from 3 cm on the CT obtained two months previously (Figure 2). The appearance was most suggestive of a bronchocele.

Figure 2: Repeat CTPA.
The same day, the patient underwent a bronchoscopy that demonstrated findings consistent with a pink smooth-walled vascular mass consistent with carcinoid tumor in the right lower lobe (Figure 3). Transbronchial biopsies surprisingly revealed fragments of moderately differentiated squamous cell carcinoma (Figure 4a). Staging of the malignancy was consistent with T2, N0, and M0. Immunohistochemistry showed positive staining of the neoplastic cells for p63 (Figure 4b). CK7, CK20, PSA, and PSAP were all negative. The patient was referred to the rapid access lung clinic. Due to multiple co-morbidities, the patient was not deemed to be a suitable surgical candidate and subsequently commenced radiation therapy.

Figure 3: Bronchoscopy image.
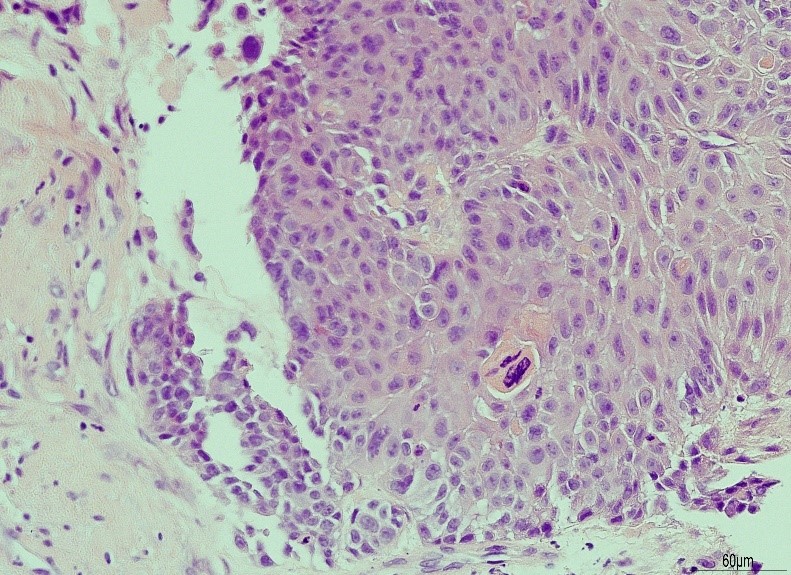
Figure 4a: Histology.
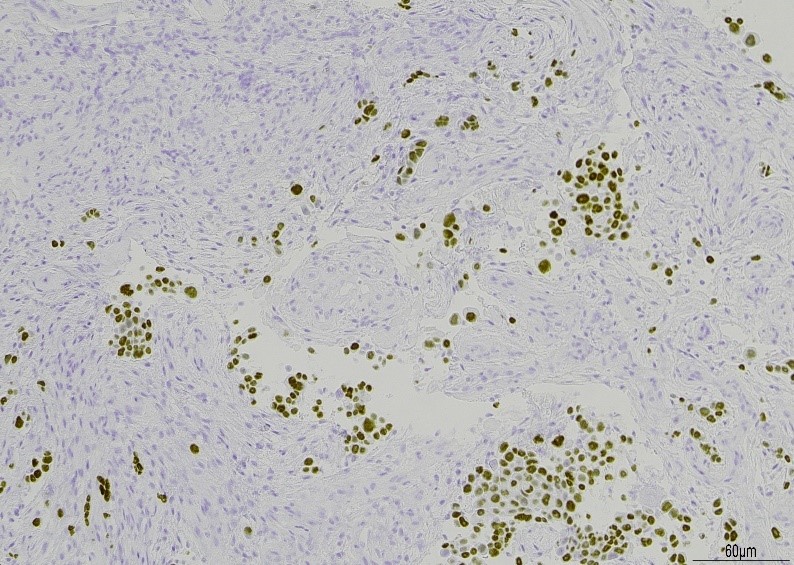
Figure 4b: p63 staining.
Discussion
Bronchoceles diagnosed radiologically can mimic many different pathologies. A recent case report in the “American Journal of Case Reports” described a bronchial carcinoid that radiologically had the appearance of a bronchocele [1]. Another recent case report described an 84-year-old female patient who presented with a cough on a background history of a surgical resection of a colorectal mucinous adenocarcinoma. CT demonstrated the appearance of a lobulated elongated lesion consistent with a bronchocele. On bronchoscopy, there was obstruction of the right muddle lobe by solid green-yellow tissue; endobronchial biopsy confirmed mucinous colorectal adenocarcinoma [2]. Another case report in the Journal of Thoracic Oncology described the resection of a solitary pulmonary metastasis from prostatic adenocarcinoma misdiagnosed as a bronchocele [3]. A case of endobronchial TB and several cases of congenital bronchial atresia have been described [4-6].
Conclusions
In rare cases, neoplasms have been associated with bronchoceles emphasising the importance of bronchoscopy (for direct visualisation) and biopsy in the workup. This case describes an unusual presentation of a squamous cell lung carcinoma which had the radiographic appearance of a bronchocele and the semblance of a carcinoid tumour, on direct visualization via bronchoscopy; however, biopsy confirmed the diagnosis of a moderately differentiated squamous cell carcinoma.
References
1. Howlader N, Noone AM, Krapcho M, et al. editors. SEER Cancer Statistics Review, 1975-2008. Bethesda (MD): National Cancer Institute; 2010. Available at: https://bit.ly/2ZnCC2n
2. Saadé-Yordán C, McBurney-Henriquez E, González-Santoni R, et al. 2017. Marked 18-Fuorine-Fluorodeoxyglucose (FDG) Avidity of an Intrapulmonary Typical Carcinoid Tumor Manifesting as a Bronchocele in an Asymptomatic Middle-Aged Woman Am J Case Rep. 18: 1390-1395. Ref.: https://bit.ly/2KfsPb9
3. Balata H, Evison M, O'Donnell P. 2015. Beware of the "Bronchocele," Particularly in Patients with a History or Risk Factors for a Mucinous Carcinoma: A Response to the Article "Resection of a Solitary Pulmonary Metastasis from Prostatic Adenocarcinoma Misdiagnosed as a Bronchocele: Usefulness of 18F-Choline and 18F-FDG PET/CT" by Calais et al. J Thorac Oncol. 10: 47-48.
4. Calais J, Lussato D, Menard J, et al. 2014. Resection of a solitary pulmonary metastasis from prostatic Adenocarcinoma misdiagnosed as a Bronchocele: usefulness of 18F-choline and 18F-FDG PET/CT. J Thorac Oncol. 9. Ref.: https://bit.ly/2MKGDg2
5. Singh H, Jetley RK, Maurya V, et al. 2001. Endobronchial tuberculosis presenting as a bronchocele. Med J Armed Forces India. 57. 68-69. Ref.: https://bit.ly/2ZiMIBH
6. Bronchocele: Two Cases, Gulfidan Cakmaka, Nurdan Gockunb, Emre Evrenb, Zuhal Aydan Saglamc. J Med Cases. 2013; 4: 594-597.




















