Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/jcri.2022.110034Article Views : 0Article Downloads : 1
Single centre experience of TEVAR for traumatic aortic transection
Masooma Asghar Ali Juma*
King Khaled Hospital Najran, KSA
*Corresponding Author: Masooma Asghar Ali Juma, King Khaled Hospital Najran, KSA; Email: somee.sa7@gmail.com
Article Information
Aritcle Type: Case Report
Citation: Masooma Asghar Ali Juma. 2022. Single centre experience of TEVAR for traumatic aortic transection. J Case Rept Img. 4: 32-39.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2022; Masooma Asghar Ali Juma
Publication history:
Received date: 04 October, 2022Accepted date: 11 October, 2022
Published date: 13 October, 2022
Abstract
Background: Traumatic aortic transection represents the second most common cause of death due to blunt trauma and thoracic endovascular aortic repair (TEVAR) has become the modality of choice to treat such injuries if the facility is available. There are many international case series available presenting their single centre experiences of TEVAR but there is lack of data from our region, although TEVAR is being used as a definitive option for the management of such patients.
Method: Reterospective review of the patients was done who underwent TEVAR between JUNE 2018 and DECEMBER 2021,. Data collection was done based on patient’s age, gender, hemodynamic stability, mechanism of injury, associated injuries, grade of injury, type of anesthesia received and procedure related complications including, paraplegia, endoleak, device migration, limb ischemia, sepsis, hospital stay, stroke and mortality. Data was analysed using spss version 28.
Results: A total of 19 patients were included in the study. All were male with mean age of 39.95 years. 94.7% patients had history of road traffic accident (RTA) and 17 out of 19 patients were hemodynamically stable at the time of presentation. Mostly patients had grade 3 aortic transection (84.2%). Mean hospital stay of patients was observed to be 13 days. Out of 19 patients, 17 patients (89.5%) had no endoleak or device migration. No limb ischemia, paraplegia, stroke, sepsis and mortality was observed in 18 patients (94.7%) during their hospital stay.
Conclusion: The results of this study are comparable to international published studies but continued surveillance and long term follow up is crucial to determine the fate of patients after discharge who underwent TEVAR at our centre.
Keywords: Traumatic Aortic Transection; Thoracic Endovascular Aortic Repair; Blunt Traumatic Thoracic Injury; Road Traffic Accidents; Interventional Radiology
Introduction
The incidence of aortic transaction is 1.5 to 2% in patients who sustain blunt thoracic trauma. It represents the second most common cause of death due to blunt trauma [1-19]. Upto 80% of patients have associated injuries. The survival of patients following a traumatic aortic injury depends on early recognition, rapid diagnosis, and prompt management. Prehospital mortality is 75 % to 80%, while in hospital mortality is 50% within 24 hours if left untreated. Only 10 % to 15 % of injured people reach a hospital alive [2,17,18]. Survival of patients depend upon the skill and judgement of the cardiothoracic surgeon and multidisciplinary team as it poses greatest difficulty for the surgeon to diagnose it [8]. Isthmus is most commonly involved in aortic transection because the ligamentum arteriosum and intercostal arteries anchor the upper descending thoracic aorta to the thorax, as do the thoracic exits of the brachiocephalic vessels. These structures decelerate with the thorax, but the distal end of the aortic arch and most proximal part of the descending thoracic aorta continue to move forward. Aortic disruption tends to develop at the interface between these two areas in this deceleration model [8]. There are many other theories which are believed to be involved in the mechanism of aortic transection namely osseous pinch, whiplash effect and water hammer effect [16]. Less commonly involved sites include arch, ascending aorta and descending aorta [3].
According to the azizzadeh et al. Grading scale, intimal irregularities of the thoracic aorta can be classifed as grade 1 injuries, intramural hematomas as grade 2, pseudoaneurysms as grade 3 and ruptures with free extravasation as grade 4 [12]. Hemodynamically unstable trauma patients warrant emergent exploration. If blunt thoracic aortic injury is the source of instability, then immediate repair is indicated. If aortic injury is not the source of life-threatening bleeding, then delayed aortic repair (damage control approach) is safe and effective approach [20]. Management is based upon advanced Trauma Life Support (ATLS) guidelines and Thoracic Endovascular Aortic Repair (TEVAR) has become the modality of choice if the facility is available. It involves the placement of modular graft components via the iliac or femoral arteries to line the thoracic aorta and exclude the injury. It is less invasive with lower early mortality and lower occurrence of paraplegia. It avoids thoracotomy, aortic clamping and left heart bypass or cardio-pulmonary bypass (CPB) but requires expeditious imaging, trained personnel and availability of endografts [7,8]. There are many international case series available [2-5], presenting their single centre experiences of TEVAR but there is lack of data from our region, although TEVAR is being used a definitive treatment of choice for the management of patients with traumatic aortic transection.
Methods
Ethical approval was obtained from institutional review board (IRB) and scientific committe of our hospital to commence the research. Data of patients who underwent TEVAR from june 2018 to december 2021 with traumatic aortic transaction was reviewed retrospectively. Those who underwent surgical repair, got medical treatment and had abnormal arch anatomy were excluded from the study. Data collection was done from record review of patients from oasis hospital system based on patient’s age, gender, hemodynamic stability, mechanism of injury, associated injuries, grade of injury, type of anesthesia received and procedure related complications including, paraplegia, endoleak, device migration, limb ischemia, sepsis, stroke, vascular access site complications, hospital stay and mortality.
All patients were initially managed according to the advanced trauma life support (ATLS) guidelines. The initial evaluation was followed by computed tomography (CT) scan according to our trauma protocol, including a CT scan of the head, spine, chest and abdomen, and further specific radiological examinations whenever necessary. The patients were evaluated by a team of trauma, cardiothoracic surgeon, anesthesiologist, and interventional radiologist. The aortic injury was characterized with respect to the location, diameter and length of the lesion, along with concomitant injuries, so as to decide the timing of the TEVAR. In patients with concurrent injuries that were considered to be more lifethreatening than that of the aorta, those were managed prior to TEVAR. After multidisciplinary discussion, the patient subsequently underwent TEVAR. Arterial access was established through percutaneous route in all patients and the stent grafts were deployed over a stiff wire. In all patients the TEVAR was performed in hybrid OR under conscious sedation if the patient was not intubated. Cerebrospinal fluid drainage was not used in any patient, and none of the patient underwent a cervical debranching operation before stent graft insertion. Heparinization was individualized based on the risk of bleeding, concomitant injuries and complexity of the procedure. After the procedure was completed, a digital subtraction angiography was performed to verify the correct positioning of the stent and to detect any primary endoleak.
Data was analysed using spss version 28. Categorical variables including age and length of hospital stay were analysed by mean and stardard deviation, while continous variables including gender, hemodynamic stability, mechanism of injury, associated injuries, grade of injury, type of anesthesia received, paraplegia, endoleak, device migration, limb ischemia, sepsis, stroke, vascular access site complications and mortality were estimated by frequency (percentage). Patients were followed up for development of complications until admitted in the hospital by physical examination and CT angiogram of the chest.
Table1: Associated injures
|
Associated injuries |
No of patients |
Frequency (percentage) |
|
1. Lower limb bone fractures |
5 |
26.3 |
|
2. Rib fractures |
10 |
52.6 |
|
3. Lung contusions |
8 |
42.1 |
|
4. Abdominal organ injury |
7 |
36.8 |
|
5. Head injury |
1 |
5.3 |
|
6. Vertebrae fractures |
7 |
36.8 |
|
7. Pneumo/hemothorax |
9 |
47.4 |
|
8. Facial bones fracture |
1 |
5.3 |
|
9. Paraplegia |
2 |
10.5 |
|
10. Clavicle fracture |
3 |
15.8 |
|
11. Foot drop |
1 |
5.3 |
|
12. Tongue laceration |
1 |
5.3 |
|
13. Retroperitoneal hematoma |
1 |
5.3 |
|
14. Pelvic bones fracture |
2 |
10.5 |
|
15. Scapula fracture |
3 |
15.8 |
|
16. Sternal bone fracture |
1 |
5.3 |
|
17. Mandible fracture |
1 |
5.3 |
|
18. Hand bones fracture |
1 |
5.3 |
|
19. Upper limb bones fracture |
5 |
26.3 |
|
20. Pulmonary embolism |
1 |
5.3 |
Results
During the study period, a total of 19 patients underwent TEVAR for traumatic aortic transection. 17 patients had transection at the level of isthmus(89.5%), 1 patient at the level of arch and isthmus(5.3%) and 1 patient at the level of D8/D9 (5.3%). Mean age was found to be 39.95 +/- 15.3 years and all patients were male. 18 patients (94.7%) had history of road traffic accident (RTA) while 1 patient (5.3%) presented with history of fall from height. 17 out of 19 patients were hemodynamically stable at the time of presentation(89.5%), whereas 2 patients (10.5%) were unstable. Loss of consciousness was observed only in 3 patients ( 15.8%). 16 patients presented with grade 3 injury (84.2%) ( Figure 1) and 3 patients with grade 2 injury (15.8%). Mean hospital stay of patients was observed to be 13 days mainly because of the management of concomitant injuries. 1 patient (5.3%) after hospital stay of 1 day, was reffered to other centre for management of associated injuries (whose facility was not available in the hospital) so endoleak, device migration, limb ischemia, paraplegia, stroke, sepsis and mortality status of that patient is not known. 1 patient (5.3%) refused to underwent follow up CT scan with contrast. Out of 19 patients, 17 patients had no endoleak or device migration (89.5%).
No limb ischemia, paraplegia, stroke, sepsis and mortality was observed in 18 patients ( 94.7%) during their hospital stay. 1 patient had iatrogenic femoral artery injury while gaining access to the femoral artery percutaneously for TEVAR which was subsequently repaired by vascular surgeon. 1 patient with previous history of RTA was readmitted after 33 days, had type 1 endoleak. He was restented with 28mm*150mm TAG graft but later died because of gastrointestinal bleeding. Frequencies of associated injuries are presented in Tabe 1.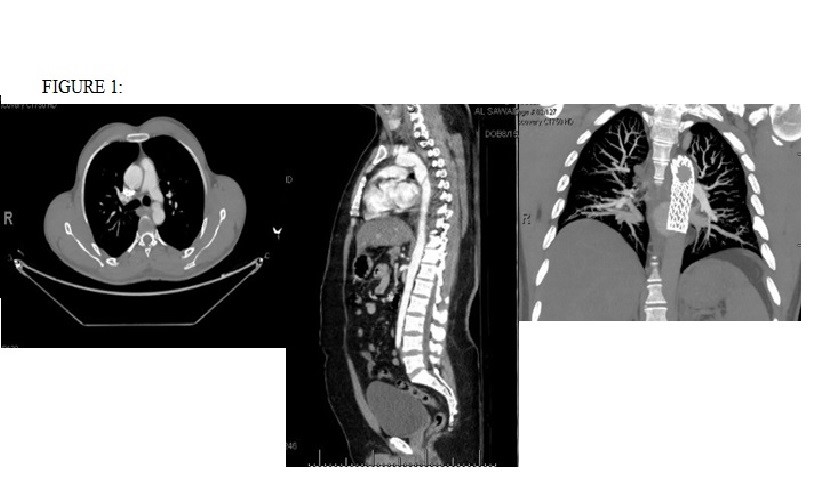
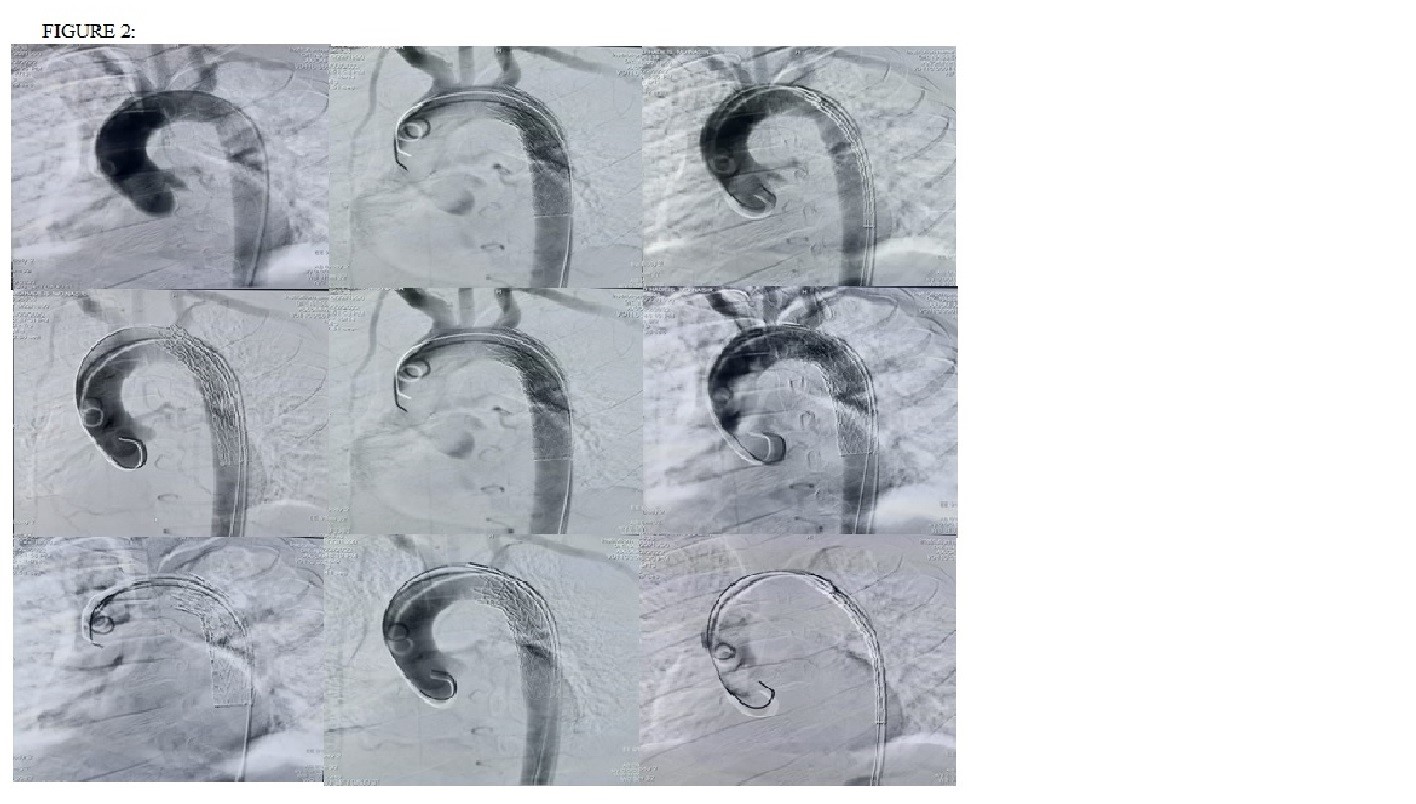
At our institute the most commonly observed associated injury with traumatic aortic transection was rib fractures ( 52.6%) followed by lung contusions 42.1% and abdominal organ injury 36.8%. Graft size in all the 12 patients was 26mm*100mm TAG, 5 patients had 28mm*100mm TAG, 1 patient had 24mm*4.9 cm B graft from Bently and 1 patient had 21 mm*100mm TAG graft. Figure 2 is showing various clips of TEVAR done in our patients.
Discussion
In recent years there has been a paradigm shift from open repair to TEVAR as the preferred treatment for patients with blunt traumatic thoracic aortic injury, regardless of patient age because of lower mortality rate as compared to open repair. Lee et al demonstrated 9% mortality rate for TEVAR as compared to open repair 19% [7]. Adequate preoperative measurements are critical for the correct sizing of thoracic endografts, and are best facilitated by computed tomography angiography (CTA) with three dimensional reformatting. This provides information about the seal zones, coverage length, and tortuosity and angulation of the aorta. The commercially available thoracic stent grafts all require a 20-mm-long proximal seal zone. It is critical to obtain good apposition throughout this segment to avoid endoleak or device migration. Depending on the patient’s anatomy, it may be necessary to cover one or more of the arch branches to obtain an adequate seal. Not infrequently, coverage of the left subclavian artery is required to obtain an adequate proximal seal. Coverage of the subclavian artery without revascularization is generally well tolerated, but may lead to left arm ischemic symptoms in a minority of patients [4,5]. In this study left subclavian artery was covered with endograft in 3 patients without any negative consequences post procedure.
The distal landing zone is also critical to avoid type 1b endoleak, and also requires a 20-mm seal zone with the currently available devices. In patients with disadvantaged distal seal zones where adequate seal can only be achieved with celiac artery coverage, selective arteriogram and demonstration of an intact gastroduodenal artery providing collateral flow from the superior mesenteric artery are necessary prior to placement of TEVAR [14].
There are five different types of endoleaks. Type 1 endoleaks are leaks at the proximal or distal attachment sites. Type 2 endoleaks are caused by retrograde flow through collateral vessels into the aneurysm sac. Type 3 endoleaks are holes, defects, or separations in the stent-graft material. Type 4 endoleaks represent porous graft walls. Type 5 endoleaks have been described as being due to endotension with an enlarging aneurysm sac without a visible endoleak [13].
All patients in the current study had concomitant injuries. Fifty-one percent of patients had an associated closed head injury, forty-six percent had multiple rib fractures, and 38% have pulmonary contusions in the study of Fabian et al published in 1997 [15] while in this series head injury was found to be in only 5.3% of patients.There was no conversion to open repair in any patient. In all patients, a single stent graft was sufficient to exclude the injured part of the aorta.
Hundermarck et al and Serra et al published series of 19 and 11 patients respectively with motor vehicle accidents being the most common mechanism of injury as consistent with the present case series. Grade 3 aortic transection was observed to be the most common injury which is similar to the previously published reports [1,4]. In the series published by Hundermarck et al, 2 patients who underwent TEVAR were hemodynamically unstable (11%). Their study did not show any evidence of endoleak and limb ischemia although 1 patient had spinal cord ischemia post TEVAR. Blunt thoracic aortic injury (BTAI) related hospital mortality was 0% which is similar to the current case series while 16% in hospital mortality was observed to be due to BTAI-unrelated causes. In another case series of Serra et al, there was also no incidence of paraplegia, endoleak and limb ischemia with 0% in hospital mortality. In a study from Taiwan, in hospital mortality rate was 9% while in a study from Italy it was 24%. Vast difference in mortality rates of different institutes worldwide indicate that many factors contribute to the survival of patients after traumatic aortic transection including associated injuries, timing of repair, hemodynamics, mechanism of injury, stent availability and financial cost [1-5].
Limitations
This study has several limitations. It is retrospective case series with outcomes reviewed only within the hospital admission. There is lack of follow up of patients after discharge to dertermine the stent graft related complications and mortality. Furthermore, time lapse between traumatic aortic transection and repair was also not calculated because of limited data availability. Despite these limitations, this study is believed to provide substantial contribution to the long term analysis of outcomes post TEVAR in future.
Conclusion
The incidence of traumatic aortic transection in our region is more as compared to other centres and TEVAR is used as modality of choice to treat such injuries. The results of this study are comparable to international published studies but continued surveillance and long term follow up is crucial to determine the fate of patients after discharge who underwent TEVAR at our centre.
Declarations
Conflict of interest
The author has no competing interests to declare that are relevant to the content of this article.
Ethics approval
Ethical approval was obtained from institutional review board (IRB) with IRB registration number “KACST' KSA: H-l1-N081”, and scientific committe of our hospital to commence the research.
References
1. Hundersmarck D, van der Vliet QMJ, Winterink LM, et al. 2022. Blunt thoracic aortic injury and TEVAR: long-term outcomes and health-related quality of life. Eur J Trauma Emerg Surg. 48: 1961-1973. Ref.: https://pubmed.ncbi.nlm.nih.gov/32632630/ DOI: https://doi.org/10.1007/s00068-020- 01432-y
2. Cheng YT, Cheng CT, Wang SY, et al. 2019. Long-term Outcomes of Endovascular and Open Repair for Traumatic Thoracic Aortic Injury. JAMA Netw Open. 2. Ref.: https://pubmed.ncbi.nlm.nih.gov/30735232/ DOI: https://doi.org/10.1001/jamanetworkopen.2018 .7861
3. Steuer J, Bjorck M, Sonesson B, et al. 2015. Editor's Choice – Durability of Endovascular Repair in Blunt Traumatic Thoracic Aortic Injury: Long-Term Outcome from Four Tertiary Referral Centers. Eur J Vasc Endovasc Surg. 50: 460-465. Ref.: https://pubmed.ncbi.nlm.nih.gov/26143100/ DOI: https://doi.org/10.1016/j.ejvs.2015.05.012
4. Serra R, de Franciscis S, Grande R, et al. 2015. Endovascular repair for acute traumatic transection of the descending thoracic aorta: experience of a single centre with a 12-years follow up. J Cardiothoracic Surg. 10: 171. Ref.: https://pubmed.ncbi.nlm.nih.gov/26590963/ DOI: https://doi.org/10.1186/s13019-015- 0388-5
5. Canaud L, Marty-Ane C, Ziza V, et al. 2015. Minimum 10-year follow-up of endovascular repair for acute traumatic transection of the thoracic aorta. J Thorac Cardiovasc Surg. 149: 825-829. Ref.:https://pubmed.ncbi.nlm.nih.gov/25481655/ DOI: https://doi.org/10.1016/j.jtcvs.2014.10.113
6. Steuer J, Wanhainen A, Thelin S, et al. 2012. Outcome of endovascular treatment of traumatic aortic transaction. J Vas Surg. 56: 973-978. Ref.: https://pubmed.ncbi.nlm.nih.gov/22608791/ DOI: https://doi.org/10.1016/j.jvs.2012.03.259
7. Lee WA, Matsumura JS, Mitchell RS, et al. 2011. Endovascular repair of traumatic thoracic aortic injury: Clinical practice guidelines of the Society for Vascular Surgery. J Vasc Surg. 53: 187-192. Ref.: https://pubmed.ncbi.nlm.nih.gov/20974523/ DOI: https://doi.org/10.1016/j.jvs.2010.08.027
8. Go MR, Barbato JE, Dillavou ED, et al. 2007. Thoracic endovascular aortic repair for traumatic aortic transection. J Vasc Surg. 46: 928-933. Ref.: =https://pubmed.ncbi.nlm.nih.gov/17980279/ DOI: https://doi.org/10.1016/j.jvs.2007.06.049
9. Starnes BW, Lundgren RS, Gunn M, et al. 2012. A new classification scheme for treating blunt aortic injury. J Vasc Surg. 55: 47-54. Ref.: https://pubmed.ncbi.nlm.nih.gov/22130426/ DOI: https://doi.org/10.1016/j.jvs.2011.07.073
10. Demetriades D, Velmahos GC, Scalea TM, et al. 2008. Operative repair or endovascular stent graft in blunt traumatic thoracic aortic injuries: results of an American Association for the Surgery of Trauma Multicenter Study. J Trauma. 64: 561-570. Ref.: https://pubmed.ncbi.nlm.nih.gov/18332794/ DOI: https://doi.org/10.1097/ta.0b013e3181641bb3
11. Tehrani. 2006. Endovascular repair of thoracic aortic tears. Ann Thorac Surg. 82: 873-877. Ref.: https://pubmed.ncbi.nlm.nih.gov/16928500/ DOI: https://doi.org/10.1016/j.athoracsur.2006.04.012
12. Azizzadeh A, Keyhani K, Miller CC, et al. 2009. Blunt traumatic aortic injury: initial experience with endovascular repair. J Vasc Surg. 49: 1403-1408. Ref.: https://pubmed.ncbi.nlm.nih.gov/19497498/ DOI: https://doi.org/10.1016/j.jvs.2009.02.234
13. Rosen RJ, Green RM. 2008. Endoleak management following endovascular aneurysm repair. J Vasc Interv Radiol. 19: 37- 43. Ref.: https://pubmed.ncbi.nlm.nih.gov/18502385/ DOI: https://doi.org/10.1016/j.jvir.2008.01.017
14. Vaddineni SK, Taylor SM, Patterson MA, et al. 2007. Outcome after celiac artery coverage during endovascular thoracic aortic aneurysm repair: preliminary results. J Vasc Surg. 45: 467-471. Ref.: https://pubmed.ncbi.nlm.nih.gov/17254741/ DOI: https://doi.org/10.1016/j.jvs.2006.11.040
15. Fabian TC, Richardson JD, Croce MA, et al. 1997. Prospective study of blunt aortic injury: Multicenter Trial of the American Association for the Surgery of Trauma. J Trauma. 42: 374- 383. Ref.: https://pubmed.ncbi.nlm.nih.gov/9095103/ DOI: https://doi.org/10.1097/00005373- 199703000-00003
16. Nzewi O, Slight RD, Zamvar V. 2006. Management of blunt thoracic aortic injury. Eur J Vasc Endovasc Surg. 31: 18-27. Ref.: https://pubmed.ncbi.nlm.nih.gov/16226902/ DOI: https://doi.org/10.1016/j.ejvs.2005.06.031
17. Mouawad NJ, Paulisin J, Hofmeister S, et al. 2020. Blunt thoracic aortic injury - concepts and management. J Cardiothorac Surg. 15: 62. Ref.: https://pubmed.ncbi.nlm.nih.gov/32307000/ DOI: https://doi.org/10.1186/s13019-020- 01101-6
18. Dagenais F, Lavoie P, Bauset R, et al. 2003. Endovascular stent-graft for blunt thoracic aortic rupture: a novel and useful approach in selected cases. Can J Surg. 46: 386-389. Ref.: https://pubmed.ncbi.nlm.nih.gov/14577715/
19. Dyer DS, Moore EE, Ilke DN, et al. 2000. Thoracic aortic injury: how predictive is mechanism and is chest computed tomography a reliable screening tool? A prospective study of 1,561 patients. J Trauma. 48: 673-683. Ref.: https://pubmed.ncbi.nlm.nih.gov/10780601/ DOI: https://doi.org/10.1097/00005373- 200004000-00015
20. Chalvatzoulis E, Megalopoulos A, Trellopoulos G, et al. 2010. Endovascular repair of traumatic aortic transection. Interact Cardiovasc Thorac Surg. 11: 238-242. Ref.: https://pubmed.ncbi.nlm.nih.gov/20562197/ DOI: https://doi.org/10.1510/icvts.2010.235473




















