Indexing & Abstracting
Full Text
Review ArticleDOI Number : 10.36811/jcshd.2021.110021Article Views : 0Article Downloads : 2
Cardiac Rehabilitation Effects on Depression in Stable Heart Failure with Reduced Ejection Fraction Patients
Yasser Abdellatif, Abdelrahim Chahat, Khaled Said and Mohamed Zahran*
Department of Cardiology, Faculty of Medicine, Ain Shams University, Egypt
*Corresponding Author: Mohamed Zahran, Department of Cardiology, Faculty of Medicine, Ain Shams University, Egypt, Phone: +201111377796, Email: zahran@med.asu.edu.eg; zahrancardiology@yahoo.com
Article Information
Aritcle Type: Review Article
Citation: Yasser Abdellatif, Abdelrahim Chahat, Khaled Said, et al. 2021. Cardiac Rehabilitation Effects on Depression in Stable Heart Failure with Reduced Ejection Fraction Patients. J Cardiovasc Surg Heart Dis. 3: 10-20.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2021; Yasser Abdellatif
Publication history:
Received date: 14 June, 2021Accepted date: 06 July, 2021
Published date: 08 July, 2021
Abstract
Background: Heart failure (HF) is a growing chronic health condition affecting more than 20 million people worldwide. Symptoms of depression are a common co-morbidity affecting as many as 42% of patients with heart failure (HF) and are associated with a poor quality of life and adverse prognosis. Symptoms of depression have negative impacts not only on daily social and domestic activities, but also on hospitalization and mortality rates in HF patients. Cardiac rehabilitation has been shown to reduce the rate of mortality, improve functional capacity, and control reduced depressive symptoms and better clinical outcomes.
Objective: to investigate the impact of a 12-week completed cardiac rehabilitation program on depressive symptoms in patients with heart failure with reduced ejection fraction.
Patients and Methods: Sixty patients with stable heart failure with reduced ejection fraction (HFrEF) with mild, moderate and severe depressive symptoms were recruited between January 2018 to June 2019 at Ain Shams University hospitals and randomly assigned to whether or not receive a 12 weeks cardiac rehabilitation program. Cardiac rehabilitation program consisted of education, diet control, drug adherence, 12 weeks exercise sessions, behavioral and psychosocial management, and sexual activity education smoking cessation. All patients were personally interviewed for assessment of depression and quality of life before and after study period by Beck's depression inventory – II(BDI-II) and Minnesota living with heart failure questionnaire" (MLHFQ), respectively. Besides, all patients underwent echocardiographic assessment before and after study period.
Result: A total of 60 patients in study group were enrolled, 26 (86.7%) males in both groups. There were 22 (73.3%) patients (13 with mild depressive symptoms, 5 with moderate and 4 with severe depressive symptoms) showed significant improvement in BDI-II score (P<0.001), whereas 8 (26.7%) patients only did not improve significantly after exercise period, no patients in the study group showed worsening of his depressive symptoms after completed cardiac rehabilitation program. BDI-II score has significant positive correlation with MLHFQ score (r=0.748, P<0.001). In contrast, only 4 (13.3%) patients (all of them were having mild depressive symptoms) of control group improved significantly regarding depressive symptoms (P<0.001), and the majority of participants 16 (53.3%) patients deteriorated regarding depressive symptoms, and the rest of group 10 (33.3%) patients didn’t show significant improvement of their depressive symptoms according to BDI-II score after the 3 month study period. There was a significant difference when compared BDI-II score at baseline with score after study period for the cardiac rehabilitation group. The BDI-II score difference after study period also was significant between two groups (P <0.001).
Conclusion: The results of this study demonstrated that a complete and organized cardiac rehabilitation program improves depressive symptoms, quality of life as well as LVEF in patients with heart failure with reduced ejection fraction.
Recommendation: Cardiac rehabilitation should be implemented in routine management of patients with heart failure to improve psychological and physical complication of HF.
Keywords: Cardiac Rehabilitation; Depression; Heart Failure
Introduction
Heart failure (HF) is a growing chronic health condition affecting more than 20 million people worldwide [1]. Symptoms of depression are a common co-morbidity affecting as many as 42% of patients with heart failure (HF), and are associated with a poor quality of life and adverse prognosis [2-4]. Symptoms of depression have negative impacts not only on daily social and domestic activities, but also on hospitalization and mortality rates in HF patients [5]. Furthermore, depression has been shown to be an independent predictor of future cardiac events in patients with heart failure, regardless of disease severity, making it worthwhile to consider among other cardiac risk factors, such as diabetes mellitus and smoking [6]. Thus, a reduction in the patient's depressive symptoms has become of prime importance for therapeutic intervention. Despite recent advances in pharmacological management, however, treating the symptoms of depression is especially challenging in HF patients because they are often on complex medications besides multiple co-morbidities [2]. Non-pharmacological interventions, such as exercise training, have been demonstrated as potential treatments for depression and may be comparable with antidepressant therapy, but these effects are not well identified in patients with HF [7-9]. Exercise (as part of cardiac rehabilitation program) provides important advantages over pharmacotherapy, including fewer drug interactions and more involvement of patients in their self-care. The largest Heart Failure-A Controlled Trial Investigating Outcomes of Exercise Training (HF ACTION), demonstrated that exercise results in a modest reduction in depressive symptoms [10]. Moreover, scarce data are available in the Middle East populations in general and Egyptian patients in particular, who have different etiology, ethnic, cultural backgrounds and risk factors from those patients in the west.
Objective
The aim of this study is to investigate the impact of a 12-week cardiac rehabilitation program on depressive symptoms in patients with heart failure and reduced ejection fraction.
Patients and Methods
This study was a randomized, unblinded, prospective clinical study of cardiac rehabilitation versus usual care in patients with heart failure and reduced ejection fraction (HFrEF). Randomization was done by a computer based program randomizing the sequence of patients whether to the cardiac rehabilitation group or to the control group.
Patients included in this study were aged 18 to 65 years old with stable chronic heart failure, left ventricular ejection fraction (LVEF) ≤40%, New York Heart Association (NYHA) class II and III and Beck Depression Inventory-II (BDI-II) score ≥14. Patients with decompensated heart failure or NYHA class IV, history of depression disorder before cardiac problem or on medical antidepressant treatment, and drug abusers. Patients were recruited from the university hospital from January 2018 to June 2019. Patients with HFrEF, included in this study, were divided into 2 groups. Patients were randomly assigned in 1:1 fashion via permuted block randomization to either cardiac rehabilitation (CR) group or standard care (SC) group, the study protocol was approved by the local ethics committee and all patients provided an agreement upon a voluntary informed consent.
Clinical Data Collection
Patient characteristics were obtained including cardiac risk factors (hypertension, diabetes mellites, smoking), occupation and etiology of heart failure (ischemic or non-ischemic). Current antifailure medications (Renin-Angiotensin-Aldosterone antagonist “RAAS blocker”, B- blocker, Mineralocorticoid receptor antagonist “MRA”) were documented as medications being taken at the time of baseline assessment.
Assessment of Depression
Depression was assessed twice at baseline and after 3 months in both groups by the Beck Depression Inventory-II (BDI-II). The BDI-II has been widely studied in cardiac patients and has excellent psychometric properties including a test-retest reliability coefficient of 0.93. The BDI-II is a 21-item, self-report measure of depressive symptoms using a 0-3 scale (range 0-63) [11]. Each item tackles a particular symptom of depression. The cutoff points for different categories were as follows: minimal depression 0–13, mild depression 14–19, moderate depression 20–28 and severe depression 29–63. A score of 14 or greater is considered to reflect clinically significant depressive symptoms [11]. Thus, patients with BDI-II less than 14 were excluded from the study.
Assessment of functional capacity
Functional capacity was subjectively assessed according to NYHA functional classification at baseline and after 3 months. Patients with NYHA functional class I or IV were excluded from the study.
Assessment of Quality of life
Health-related Quality of life (HRQoL) was assessed at baseline and after 3 months in both groups with "Minnesota living with heart failure questionnaire" (MLHFQ). The MLHFQ is a self-administered disease-specific questionnaire for patients with HF, comprising 21 items rated on six-point Likert scales, representing different degrees of impact of HF on HRQoL, from 0 (none) to 5 (very much). It provides a total score (range 0–105, from best to worst HRQoL), as well as scores for two dimensions, physical (8 items, range 0–40) and emotional (5 items, range 0–25). The other eight items (of the total of 21) are only considered for the calculation of the total score [12].
Echocardiographic assessment
M-mode and two-dimensional echocardiographic studies were performed using commercially available echocardiographic machines equipped with a 2.5-MHz multifrequency phased array transducer (Philips HD11XE) in a blinded manner to study protocol by an independent experienced operator, at baseline which determined patient's eligibility and baseline measurements, and after 3 months which determined final measurements of study. Left ventricular end-diastolic volume (EDV) and end-systolic volume (ESV) were obtained from the apical 4- and 2-chamber views by a modified biplane Simpson’s rule, according to the recommendations of the American Society of Echocardiography, from which ejection fraction was automatically calculated as the difference between EDV and ESV normalized to EDV [13].
Cardiac Rehabilitation (CR) group
All patients in the CR group attended a 12-week cardiac rehabilitation program. The cardiac rehabilitation program is a comprehensive program that comprised supervised exercise training in addition to risk factor modification and patient education. Patients were exercised twice weekly for 12 consecutive weeks. Patients included in the CR group were those who were adherent to the cardiac rehabilitation program. Adherence to the program was defined as attending more than twenty exercise sessions without three consecutive missed sessions. During the sessions, besides exercise, each patient from the CR group was consulted and educated individually about the nature of his disease, cardiac risk factors and importance of both lifestyle modifications and adherence to prescribed medications. Additionally, each patient received dietary consultations and psychological support besides sexual and smoking cessation advice, where needed.
Exercise protocol
Each exercise session lasted for 45-60 minutes commencing with warm-up phase (5-10 minutes) with gradual increase in heart rate, followed by aerobic training (30 minutes) with maintenance of target heart rate and finally a cool-down phase (5-10 minutes) with gradual decrease in heart rate. During each session, the intensity of exercise, heart rate (from ECG monitoring), and blood pressure were measured at rest before exercising, at the middle of work on treadmill, and after 5 minutes of load less recovery. All sessions were held at the hospital's cardiac rehabilitation room under the supervision of a cardiologist. Exercise prescription during cardiac rehabilitation program and intensity of exercise was individualized based on patient's clinical status to achieve 40–80% of heart rate reserve (HRR), calculated from a baseline exercise testing using Modified Bruce protocol. Karvonen formula was utilized to calculate individualized target heart rate, where target HR = [HRR x % intensity desired] + baseline resting heart rate. HRR is the difference between maximum achieved heart rate and baseline resting heart rate [14].
Standard care (SC) group
Patients in the SC group received educational support according to recommendations of European society of cardiology; they were encouraged to adhere to their individually tailored cardiovascular medications and activity recommendations (but no formal exercise protocol), but to avoid any undue physical activity that caused intolerable breathlessness or fatigue.
Follow-Up and Outcome Measures
Follow-up started the day after the end of the maintenance exercise training protocol, for each patient of CR group, that is, after 3 months of exercise training. Whereas patients of SC group were followed up after 3 months from first time of collecting their clinical data and completed their BDI-II questionnaire. Follow-up ended at the time of study closure or with an adverse event. Functional capacity was reassessed subjectively at follow-up by NYHA. Both depression and HRQoL were reassessed by repeat administration of the BDI-II and MLHFQ after 3 months respectively, and LVEF was also assessed by repeat echocardiography. A previous report suggested that an approximate 50% reduction in clinical symptoms is generally considered to be clinically meaningful in trials of patients with major depression [15], thus in our study significant clinical improvement in BDI-II score was considered when it dropped below 14 or 50% reduction from baseline score was attained [16].
Statistical analysis
Data was coded and entered using SPSS program version 20. A suitable statistical test was used. Quantitative data was expressed as the mean ± standard deviation (SD). Paired t-test was used to compare between 2 groups as regards quantitative variables. Chi-square test was used to compare qualitative variables. Multiple comparisons were assessed by repeated-measures ANOVA. A value of P<0.05 was considered statistically significant. Correlations were determined using Pearson correlation coefficient for normally distributed variables.
Results
One hundred twenty-two patients with HFrEF were evaluated for possible enrollment, and completed BDI-II, of which seventy patients (42.6%) had clinically significant depressive symptoms, defined as calculated baseline BDI-II scores ≥14. The 70 participants were randomly assigned (via permuted block randomization) to either a 3-month CR program (n=35) or SC group (n=35). Five patients in the CR group were excluded because of concomitant comorbidities limiting exercise (n=2), and non-adherence to CR sessions (n=3). In the SC group, one patient died of sudden cardiac death, one month after enrollment, three patients decided to withdraw from the study after a few weeks, and another patient was admitted to hospital because of temporarily worsening dyspnea and decompensated heart failure. A total of 60 patients completed the study (30 in CR group and 30 in SC group). The baseline demographic data and clinical risk factors among both study groups are shown in (Table 1). No significant difference between both groups as regards age, gender and ischemic etiology for HFrEF. In addition, both groups were not significantly different as regards clinical risk factors, occupation, NYHA functional class, MLHFQ, BDI-II or baseline LVEF. Moreover, both groups were on HFrEF guideline-recommended antifailure medications (RAAS blockers, B-blockers or MRA) with similar adherence.
After the 3-month follow-up
After 3 months of supervised exercise, patients in the CR group were in a significantly better functional class compared to the SC group (p<0.001), besides having a significantly lower both MLHFQ and BDI-II (p<0.001). In addition, although there was no significant difference in baseline LVEF, the CR group showed a significantly higher LVEF compared to SC group (Table 2). When comparing the magnitude of change in both groups that occurred after the 3-month period, patients in CR group achieved significant points reduction in BDI-II scores (7.4± 6.5) compared to a 1.2±3.9-point increase in SC group (p=0.004), although there was no significant difference between both groups as regards baseline BDI-II. Considering clinically significant improvement in depression level, 18 (60%) patients in CR group showed a clinically significant improvement in BDI-II score, whereas only 4 (13.3%) in the SC group improved significantly. In addition, patients in the CR group achieved a significant improvement in LVEF compared to SC group (5±4.5 versus -0.40±3.8, p<0.001) (Table 3).
|
Table 1: Baseline Demographic and Clinical Characteristics of Sample. |
|||
|
|
CR group |
SC group |
P-value |
|
Demographics |
|||
|
Age (years) |
51 ±10.5 |
51.8±9.8 |
0.771 |
|
Males |
26 (86.7%) |
26 (86.7%) |
1 |
|
Etiology |
|||
|
Ischemic |
27 (90%) |
25 (83.3%) |
0.447 |
|
Risk factors |
|||
|
Hypertension |
13 (43.3%) |
12 (40%) |
0.793 |
|
Diabetes Mellites |
10 (33.3%) |
9 (30%) |
0.077 |
|
Dyslipidemia |
14 (46.7%) |
17 (56.7%) |
0.438 |
|
Smoking |
21 (70%) |
24 (80%) |
0.371 |
|
Occupation |
22 (73.3%) |
23 (76.7%) |
0.766 |
|
Clinical and echocardiographic assessment parameters |
|||
|
NYHA II |
8 (26.7%) |
14 (46.7%) |
0.108 |
|
NYHA III |
22(73.3%) |
16 (53.3%) |
|
|
MLHFQ |
49.1±13.9 |
50.7±14.45 |
0.664 |
|
BDI-II |
20.57±6.46 |
21.4±6.05 |
0.608 |
|
LVEF |
33.47±5.84 |
32.9±5.22 |
0.693 |
|
Medications |
|||
|
RAAS blocker |
26 (86.7%) |
24 (80%) |
0.488 |
|
B-blocker |
28 (93.3%) |
25 (83.3%) |
0.228 |
|
MRA |
14 (46.7%) |
18 (60%) |
0.300 |
|
Abbreviations: BDI-II: Beck Depression Inventory II; MLHFQ: Minnesota Living with Heart Failure Questionnaire; LVEF: Left Ventricular Ejection Fraction; NYHA: New York Heart Association; RAAS: Renin-Angiotensin-Aldosterone; MRA: Mineralocorticoid Receptor Antagonist |
|||
|
Table 2: Comparison between both groups after the 3-month study period |
||||
|
|
CR group |
SC group |
Test value |
P-value |
|
NYHA I |
21 (70%) |
5 (16.7%) |
21.741 |
<0.001 |
|
NYHA II |
6 (20%) |
6 (20%) |
||
|
NYHA III |
3 (10%) |
16 (53.3%) |
||
|
NYHA IV |
0 (0%) |
3 (10%) |
||
|
MLHFQ |
26.20±15.66 |
51.50±16.33 |
-6.124 |
<0.001 |
|
BDI-II |
13.20±6.19 |
22.57±6.5 |
-5.714 |
<0.001 |
|
LVEF |
38.47±5.44 |
32.50±5.25 |
4.323 |
<0.001 |
|
Table 3: Comparison of differences in 3 variables (BDI-II, MLHFQ, LVEF) between both groups |
||||
|
Differences |
CR group |
SC group |
Test value• |
P-value |
|
Beck |
-7.37±6.53 |
1.20±3.92 |
6.163 |
0.004 |
|
MLHFQ |
-22.90±12.69 |
0.80±12.04 |
7.421 |
<0.001 |
|
LVEF |
5.00±4.52 |
-0.40±3.77 |
-5.025 |
<0.001 |
Regarding MLHFQ, patients in the CR group achieved a 22.9±12.7 points reduction in MLHFQ scores compared to 0.80±12.04 points increase in SC group) after 3 months which is highly significant between 2 groups (p<0.001). On examining the correlation between the degree of change in BDI-II and degree of change in MLHFQ in the whole study population, there is a strong positive correlation between degree of improvement in depression level and quality of life (r=0.79, p<0.001) as shown in Figure 1.
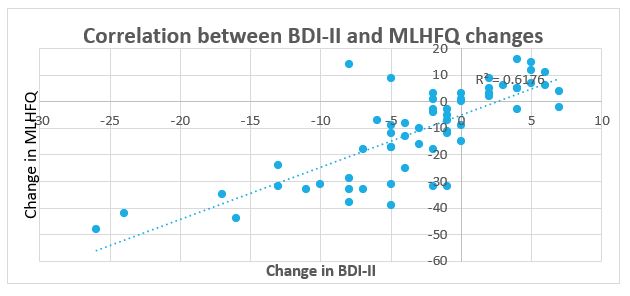
Figure 1: Correlation between the change in BDI-II and MLHFQ scores after 3 months.
Discussion
Patients with HFrEF experience progressive disability and a decline in health-related QOL. In addition to clinical derangements (fatigue, dyspnea, etc.), functional limitations and psychological distress can restrict activities because of a decline in the QOL. The results of this prospective study demonstrated that a 12-week CR is associated with a significant reduction of depressive symptoms. Furthermore, CR is feasible, safe, and effective in improving both LVEF and quality of life. This suggests that participating in CR programs produces other positive effects on patients’ well-being. Several prior studies have shown that 3-month exercise training may be comparable to antidepressant medication in reducing depressive symptoms [8,17]. However, the benefits of antidepressant medication in cardiac patients have provided mixed results. In the SADHART study, only the subgroup of patients with more severe depression appeared to benefit from sertraline [18]. Results from the SADHART-CHF trial showed that sertraline performed no better than placebo after 12 weeks of treatment, and did not improve clinical outcomes [18]. In the ENRICHD trial, patients receiving cognitive behavioral therapy (CBT) showed a 2.7-point greater reduction in BDI scores compared to usual care controls [19]. However, ENRICHD patients were clinically depressed and received treatment (CBT and anti-depressant medication) to reduce their depression. Participants in our trial were not diagnosed with major depression disorder and most were not clinically depressed. Although some studies have suggested improvement in psychological symptoms following exercise programs [20], other studies did not show such improvement [21,22]. The results of HF-ACTION ancillary study demonstrated that exercise training may be effective in reducing depressive symptoms and by further documenting the prognostic significance of depression in HF patients. While previous studies have reported that exercise is associated with reduced symptoms of depression in patients with clinical depression, HF-ACTION ancillary study was the first randomized trial to show that exercise resulted in a significant reduction in depressive symptoms in HF patients, which is consistent with our result [23,24]. After 3 months of supervised exercise, patients in the CR group achieved a 7.4±6.5 point’s reduction in BDI-II scores compared to 1.2±3.9 points increasing in SC group. This difference is likely to be associated with better social functioning and higher quality of life. While the HF-ACTION ancillary study was conducted for patients in USA, Canada and France, this is the first study to be conducted in Egypt and Middle East, a population with possibly a distinct psychological perspective in a different environment.
The effect of CR on left ventricular systolic function is controversial [25]. Studies exploring the effect of CR on left ventricular systolic function in HFrEF patients showed that LVEF either did not change [26,27], or increased [28,29]. However, a significant improvement in LVEF was achieved in the CR group. This can be explained by the beneficial effect of exercise in addition to the frequent advice and enhancing patient adherence to the medications with proven reverse remodeling effects. It was clearly demonstrated that the change in both QOL and level of depression in patients with HFrEF are strongly interrelated and the intervention in this population by CR program results in parallel improvement in both QOL, which is an important endpoint, and depression level, common comorbidity in this population. This correlation was also shown by Hooley et al in a study in outpatients with congestive heart failure [30]. In addition, in our study conducted a significant improvement in LVEF was also achieved which elaborated the multi-faceted benefits of conducting CR programs for patients with HFrEF. In this context, cardiac rehabilitation appears to be the right time to manage psychological disorders in heart failure patients. Exercise training in the context of comprehensive CR appears, therefore, to be a safe, cost-effective that can be integrated into the overall drug and non-drug management of HFrEF patients, not only to improve symptoms of depression, but also to improve quality of life and possibly left ventricular function. A number of limitations in the present study noted. First of all is the small number of patients studied, all patients were HFrEF NYHA class II and III. Therefore, the beneficial of exercise training on depression in asymptomatic HF patients (NYHA class I) and in those with more severe HF (NYHA class IV) have not been evaluated, none of the patients had major depressive symptoms, this may have affected the absolute number of points improvement on the BDI-II questionnaire. Although elderly patients represent the largest population with chronic HF, patients who are included in cardiac rehabilitation programs are currently younger than 65, it is not clear whether exercise training has the same effect in older patients (age of >65 years). In addition, most of our patients in this study were men, then we can't decide if this result has equal benefits for women too. Moreover, we can't apply this result in patients with HF with preserved or mid-range ejection fraction, because all patients included in this study had HFrEF. Patients with non-ischemic HF were small sample, when comparing with those their HF due to ischemic etiology, then benefits of exercise on depressive symptoms in this specific entity need to be addressed in further studies.
Conclusion
In conclusion, the results of this prospective, randomized study demonstrate that CR program, not only favorably influence quality of life and possibly LVEF, but it also significantly ameliorates depressive symptoms in patients with HFrEF.
Recommendations
Cardiac rehabilitation should be implemented in routine management of patients with HFrEF to improve both their physical and psychological domains.
References
1. Ghosh RK, Ball S, Prasad V. 2016. Depression in heart failure: Intricate relationship, pathophysiology and most updated evidence of interventions from recent clinical studies. International Journal of Cardiology. 224: 170-177. Ref.: https://pubmed.ncbi.nlm.nih.gov/27657469/ DOI: https://doi.org/10.1016/j.ijcard.2016.09.063
2. Rutledge T, Reis VA, Linke SE. 2006. Depression in heart failure: a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. Journal of the American college of Cardiology. 48: 1527-1537. Ref.: https://pubmed.ncbi.nlm.nih.gov/17045884/ DOI: https://doi.org/10.1016/j.jacc.2006.06.055
3. Sherwood A, Blumenthal JA, Hinderliter AL, et al. 2011. Worsening depressive symptoms are associated with adverse clinical outcomes in patients with heart failure. Journal of the American College of Cardiology. 57: 418-423. Ref.: https://pubmed.ncbi.nlm.nih.gov/21251581/ DOI: https://doi.org/10.1016/j.jacc.2010.09.031
4. Lesman?Leegte I, van Veldhuisen DJ, Hillege HL. 2009. Depressive symptoms and outcomes in patients with heart failure: data from the COACH study. European journal of heart failure. 11: 1202-1207. Ref.: https://pubmed.ncbi.nlm.nih.gov/19926602/ DOI: https://doi.org/10.1093/eurjhf/hfp155
5. Moraska AR, Chamberlain AM, Shah ND, et al. 2013. Depression, healthcare utilization, and death in heart failure: a community study. Circulation: Heart Failure. 6: 387-394. Ref.: https://pubmed.ncbi.nlm.nih.gov/23512984/ DOI: https://doi.org/10.1161/circheartfailure.112.000118
6. Newhouse A, Jiang W. 2014. Heart failure and depression. Heart failure clinics. 10: 295-304.
7. Cooney G, Dwan K, Greig C, et al. 2013. Exercise for depression Cochrane Database. Syst Rev. 9: CD004366. Ref.: https://pubmed.ncbi.nlm.nih.gov/24026850/ DOI: https://doi.org/10.1002/14651858.cd004366.pub6
8. Blumenthal JA, Babyak MA, Doraiswamy PM, et al. 2007. Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosomatic medicine. 69: 587. Ref.: https://pubmed.ncbi.nlm.nih.gov/17846259/ DOI: https://doi.org/10.1097/psy.0b013e318148c19a
9. Herring MP, Puetz TW, O’Connor PJ. 2012. Effect of exercise training on depressive symptoms among patients with a chronic illness: a systematic review and meta-analysis of randomized controlled trials. Archives of Internal Medicine. 172: 101-111. Ref.: https://pubmed.ncbi.nlm.nih.gov/22271118/ DOI: https://doi.org/10.1001/archinternmed.2011.696
10. Blumenthal JA, Babyak MA, O’Connor C, et al. 2012. Effects of exercise training on depressive symptoms in patients with chronic heart failure: the HF-ACTION randomized trial. Jama. 308: 465-474. Ref.: https://pubmed.ncbi.nlm.nih.gov/22851113/ DOI: https://doi.org/10.1001/jama.2012.8720
11. Beck AT, Steer RA, Brown GK. 1996. BDI-II: Beck depression inventory. Pearson.
12. Rector TS, Cohn JN. 1992. Assessment of patient outcome with the Minnesota Living with Heart Failure questionnaire: reliability and validity during a randomized, double-blind, placebo-controlled trial of pimobendan. American heart journal. 124: 1017-1025. Ref.: https://pubmed.ncbi.nlm.nih.gov/1529875/ DOI: https://doi.org/10.1016/0002-8703(92)90986-6
13. Lang RM, Badano LP, Mor-Avi V, et al. 2015. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. European Heart Journal-Cardiovascular Imaging. 16: 233-271. Ref.: https://pubmed.ncbi.nlm.nih.gov/25712077/ DOI: https://doi.org/10.1093/ehjci/jev014
14. Karvonen MJ. 1957. The effects of training on heart rate: A longitudinal study. Ann Med Exp Biol Fenn. 35: 307-315. Ref.: https://pubmed.ncbi.nlm.nih.gov/13470504/
15. Frank E, Prien RF, Jarrett RB, et al. 1991. Conceptualization and rationale for consensus definitions of terms in major depressive disorder: remission, recovery, relapse, and recurrence. Archives of general psychiatry. 48: 851-855. Ref.: https://pubmed.ncbi.nlm.nih.gov/1929776/ DOI: https://doi.org/10.1001/archpsyc.1991.01810330075011
16. Reeves GM, Rohan KJ, Langenberg P. 2012. Validation of BDI-II response and remission cut-points for assessment of seasonal affective disorder patients. Journal of affective disorders. 138: 123. Ref.: https://pubmed.ncbi.nlm.nih.gov/22277151/ DOI: https://doi.org/10.1016/j.jad.2011.12.003
17. Blumenthal JA, Babyak MA, Moore KA, et al. 1999. Effects of exercise training on older patients with major depression. Archives of internal medicine. 159: 2349-2356.
18. Glassman A, O’Connor C, Califf R, et al. 2002. Sertraline Antidepressant Heart Attack Randomized Trial (SADHEART) Group. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 288: 701-709. Ref.: https://pubmed.ncbi.nlm.nih.gov/12169073/ DOI: https://doi.org/10.1001/jama.288.6.701
19. Berkman LF, Blumenthal J, Burg M, et al. 2003. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. JAMA. 289: 3106-3116. Ref.: https://pubmed.ncbi.nlm.nih.gov/12813116/ DOI: https://doi.org/10.1001/jama.289.23.3106
20. Klocek M, Kubinyi A, Bacior B. 2005. Effect of physical training on quality of life and oxygen consumption in patients with congestive heart failure. International journal of cardiology. 103: 323-329. Ref.: https://pubmed.ncbi.nlm.nih.gov/16098397/ DOI: https://doi.org/10.1016/j.ijcard.2004.10.021
21. Miche E, Roelleke E, Wirtz U, et al. 2008. Combined endurance and muscle strength training in female and male patients with chronic heart failure. Clinical Research in Cardiology. 97: 615-622. Ref.: https://pubmed.ncbi.nlm.nih.gov/18432395/ DOI: https://doi.org/10.1007/s00392-008-0660-y
22. Dracup K, Evangelista LS, Hamilton MA, et al. 2007. Effects of a home-based exercise program on clinical outcomes in heart failure. American heart journal. 154: 877-883. Ref.: https://pubmed.ncbi.nlm.nih.gov/17967593/ DOI: https://doi.org/10.1016/j.ahj.2007.07.019
23. Mead GE, Morley W, Campbell P. 2008. Exercise for depression. Cochrane database of systematic reviews. 2008.
24. Lawlor DA, Hopker SW. 2001. The effectiveness of exercise as an intervention in the management of depression: systematic review and meta-regression analysis of randomised controlled trials. Bmj. 322: 763. Ref.: https://pubmed.ncbi.nlm.nih.gov/11282860/ DOI: https://doi.org/10.1136/bmj.322.7289.763
25. Haykowsky MJ, Liang Y, Pechter D. 2007. A meta-analysis of the effect of exercise training on left ventricular remodeling in heart failure patients: the benefit depends on the type of training performed. Journal of the American College of Cardiology. 49: 2329-2336. Ref.: https://pubmed.ncbi.nlm.nih.gov/17572248/ DOI: https://doi.org/10.1016/j.jacc.2007.02.055
26. Sullivan MJ, Higginbotham MB, Cobb FR. 1988. Exercise training in patients with severe left ventricular dysfunction. Hemodynamic and metabolic effects. Circulation. 78: 506-515. Ref.: https://pubmed.ncbi.nlm.nih.gov/3409495/ DOI: https://doi.org/10.1161/01.cir.78.3.506
27. McKelvie RS, Teo KK, Roberts R, et al. 2002. Effects of exercise training in patients with heart failure: the Exercise Rehabilitation Trial (EXERT). American heart journal. 144: 23-30. Ref.: https://pubmed.ncbi.nlm.nih.gov/12094184/ DOI: https://doi.org/10.1067/mhj.2002.123310
28. Erbs S, Linke A, Gielen S, et al. 2003. Exercise training in patients with severe chronic heart failure: impact on left ventricular performance and cardiac size. A retrospective analysis of the Leipzig Heart Failure Training Trial. European Journal of Cardiovascular Prevention & Rehabilitation. 10: 336-344. Ref.: https://pubmed.ncbi.nlm.nih.gov/14663295/ DOI: https://doi.org/10.1097/01.hjr.0000099031.38268.27
29. Giannuzzi P, Temporelli PL, Corrà U. 2003. Antiremodeling effect of long-term exercise training in patients with stable chronic heart failure: results of the Exercise in Left Ventricular Dysfunction and Chronic Heart Failure (ELVD-CHF) Trial. Circulation. 108: 554-559. Ref.: https://pubmed.ncbi.nlm.nih.gov/12860904/ DOI: https://doi.org/10.1161/01.cir.0000081780.38477.fa
30. Hooley PJD, Butler G, Howlett JG. 2005. The Relationship of Quality of Life, Depression, and Caregiver Burden in Outpatients with Congestive Heart Failure. Congestive Heart Failure. 11: 303-310. Ref.: https://pubmed.ncbi.nlm.nih.gov/16330905/ DOI: https://doi.org/10.1111/j.1527-5299.2005.03620.x




















