Indexing & Abstracting
Full Text
Research ArticleDOI Number : 10.36811/gju.2019.110001Article Views : 5719Article Downloads : 44
Iatrogenic Ureterovaginal Fistulae: Difficulties in Diagnosis and Treatment in Our Case series
Cristina Palmer, DO; Bilal Farhan, MD and Gamal Ghoniem, MD FACS*
Department of Urology, University of California, Irvine, USA
*Corresponding author: Gamal Ghoniem, MD FACS, Department of Urology, University of California, Irvine, USA, Email: gghoniem@uci.edu
Article Information
Aritcle Type: Research Article
Citation: Cristina Palmer, DO Bilal Farhan, Gamal Ghoniem. 2019. Iatrogenic Ureterovaginal Fistulae: Difficulties in Diagnosis and Treatment in Our Case series. Glob J Urol. 1: 01-06.
Copyright: This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2019; Cristina Palmer
Publication history:
Received date: 23 February, 2019Accepted date: 06 March, 2019
Published date: 08 March, 2019
Introduction
Ureteral injury is a known complication of pelvic surgeries, including gynecological, urologic, colorectal, and vascular surgeries. This can occur by transvaginal, laparoscopic, or transabdominal approach [1,2]. Gynecological surgery remains by far the most common means of injury (75%), followed by colorectal surgeries (14%) [3-5], with reports of ureteral injury during gynecologic surgery from 0.35% to 1.5% [4,6]. Total abdominal and laparoscopic hysterectomies are the most common procedures where ureteral injury occurs [1,5]. Injury occurs most often at the level where the ureter courses under the uterine vessels, followed by the ureterovesical junction and the base of the infundibulopelvic ligament [4,7,8]. Many ureteral injuries occur during uncomplicated, routine surgery [8,9].
An abnormal connection between the ureter and vagina, or ureterovaginal fistula, allows for a conduit through which urine can continually leak. This is specific to the combination of ureteral injury and hysterectomy where the urine finds its way to the freshly closed vaginal cuff. Genitourinary fistula formation remains one of the most feared complications of pelvic surgery, with lasting emotional damage, risk for infections, infertility, reoperation, and increased hospital stay [5,10]. Our objective is to present the difficulties encountered in management of our cases and how to rectify them.
Materials and Methods
A total of four cases of ureterovaginal fistulas were treated at our institution between 2011 and 2017. The average age of our patients was 49 (range 44-58). All ureteral injuries were not recognized at the time of surgery. The etiology of the injury was a laparoscopic assist robotic hysterectomy in three patients, two for gynecological cancer, one for fibroid disease. One patient underwent an open radical hysterectomy for cervical carcinoma, with a concomitant uterosacral vault suspension, retropubic sling, and perineoplasty. Three patients presented 4-6 weeks postoperatively with leakage of urine per vagina. These three patients were diagnosed with CT urogram. One patient presented one month postoperatively with fever, abdominal distention, and acute kidney injury, reporting leakage from vagina since the day of her robotic hysterectomy. She was found to have unrecognized bilateral ureteral injuries, with a right ureterovaginal fistula, diagnosed by retrograde pyelogram.
Results
The three patients with unilateral ureteral injury with development of ureterovaginal fistula underwent placement of percutaneous nephrostomy tubes. One patient was then treated with ureteral stent placement for a duration of four months, after which, retrograde pyelogram demonstrated resolution of the fistula. Two patients were treated with open neoureterocystotomy with Boari flap and placement of stent. The patient with bilateral ureteral injury was treated with open bilateral neoureterocystotomy, closure of ureterovaginal fistula, and psoas hitch. All patients in our series had renal preservation. Postoperatively, stents were removed in 2-6 weeks, depending if the patient had undergone external beam radiation in the past. Their postop follow up ranges 2 months to 3 years. No patient has required retreatment or intervention to date. We strongly advocate for tension-free anastomosis with absorbable sutures, over a stent, as well as use of omental or peritoneal interposition, if possible.
Discussion
Pathogenesis and Prevention
Risk factors for formation of ureterovaginal fistula include endometriosis, malignancy of the pelvis, a history of radiation therapy, obesity, and pelvic inflammatory disease [5]. Ureterovaginal fistulae may occur as a result of unrecognized [11] intraoperative laceration, thermal injury, obstruction due to ligation, or from compromise to the blood supply, resulting in ischemic necrosis [5]. In post-hysterectomy cases decrease of vaginal urinary leakage from the cuff is usually an indication of pelvic urinoma causing fibrosis which usually extends to the proximal end of the ureter. Ureteral wall becomes affected and obstruction can be seen even more proximal than the injury site. The pelvic ureter becomes also adherent to the iliac vessels. More over the pelvic urine extravasation leads to severe adhesions of both large and small bowels, making future repair and dissection very difficult and hazardous.
Meticulous dissection, knowledge of pelvic anatomy, and direct visualization of the ureter remain the most effective methods to avoid ureteral injury. The use of prophylactic ureteral catheters have not been found to decrease ureteral injury intraoperatively [3]. More recently, lighted ureteral stents as well as intraureteral injection of indocyanine green, combined with near-infrared light have been used to identify the ureter intraoperatively in laparoscopic and robotic surgeries [12]. A meticulous, hemostatic surgical field decreases the risk for ureteral injury, as well as ligating small pedicles when coming across the ureterosacral and transverse uterterine ligaments [4].
Diagnosis
Although immediate recognition and repair is preferred, ureteral injury is most often diagnosed postoperatively, with 60% requiring reoperation [9,11]. Ureteral injury is identified only 11-12% of the time intraoperatively without cystoscopy [8]. Ureteral obstruction may cause flank pain or be asymptomatic. The patient may develop a urinoma, hematuria, peritonitis, fever, renal failure, or ileus prior to fistula formation [11]. As the ureterovaginal fistula presentation is most often delayed, the patient may report normal voiding patterns with thin, watery vaginal discharge or continuous leakage postoperatively [9,11].
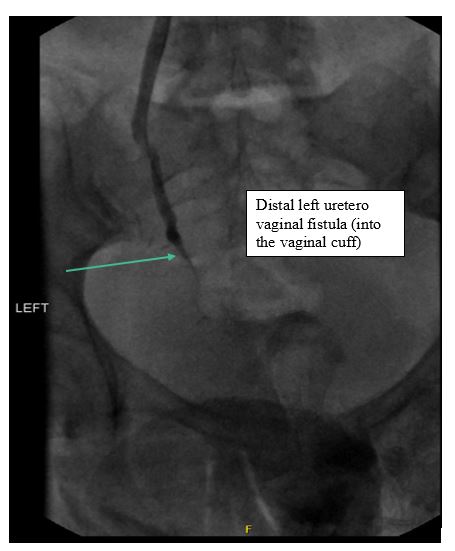
Multidetector computed tomography (MDCT) remains the gold standard for detection of ureteral injuries, especially in delayed diagnoses. Delayed contrast imaging (CT urogram) (Figure 1) is effective to detect location of injury, contrast extravasation, fistula formation, and any if any hydronephrosis or concomitant urinoma exists [8,9,13]. Antegrade and reterograde pyelography is also useful in delineating location of the injury (Figure 2), and is successful in diagnosing stricture or obstruction [9,11]. Magnetic resonance imaging may be used to localize small fistulae near the trigone [14].
A history of pelvic surgery combined with change in clinical condition and vaginal discharge should raise question of fistula formation. A comprehensive history and physical can aid in diagnosis. Traditionally, a double dye test has been performed when clinical suspicion of fistula is high, to distinguish between vesicovaginal and ureterovaginal fistula. The patient is administered oral phenazopyridine, which turns the urine orange. A tampon is placed in the vagina. The bladder is then retrograde filled with methylene blue or indigo carmine. A tampon which turns orange at the proximal portion is suggestive of a ureterovaginal fistula and distal blue staining indicates the presence of a vesicovaginal fistula [8,11].
Figure 1: Delay film of CT urogram showing fistula tract distal left ureter and vaginal cuff(arrow).

Figure 2: left antegrade nephrostogram showed the distal left uerterovaginal fistula.
Management
The delayed diagnosis of ureterovaginal fistulae can lead to ureteral stricture, renal damage, and infection [8], as seen in our patients. Patients who are candidates for conservative management are those with ureteral continuity, unilateral injury, no upper tract infection, in addition to those who are compliant with follow up [8,15,16]. In case reports, ureteral stenting has been found to be successful in fistula resolution 63-71% of the time, with a 6-38% risk of ureteral stricture [8,17]. However, stenting past the fistula is often difficult [8]. In a large case series of 84 patients, stenting past the fistula was only feasible in 9% [18]. As with our patients, placement of percutaneous nephrostomy tube is an effective temporizing measure while awaiting definitive management, however when used as a solitary method for management, has high rates for persistent fistula and stricture formation [19,20]. In the cases of failed conservative management, surgical management is dictated. Timing of repair is extremely important. It is preferable to plan the repair after three months, once the ureterovaginal fistula is diagnosed, percutaneous nephrostomy will aid to preserve renal function and decrease urine extravasation into the pelvis and vagina. Techniques for repair include transection above the diseased segment of ureter, with ureteroneocystotomy, often with concomitant psoas hitch or Boari flap [8,21]. If renal preservation is not feasible, nephrectomy may be necessary. None of our patients required this option.
Conclusion
While an uncommon complication of pelvic surgery, ureterovaginal fistulae have a significant impact on quality of life and patients may be at risk for infection or renal damage. We advocate for initial conservative measures for drainage and renoprotection, such as stent or nephrostomy tube placement. If these are unsuccessful, then referral to high volume center for reconstructive surgery is recommended.
References
- McVary K, Marshall FF. 2002. Urinary fistulae. Philadelphia: Lippincott Williams and Wilkins.[Ref.]
- ES R. 2012. Urinary tract fistulae. Philadelphia: Elsevier Saunders.[Ref.]
- Chou MT, Wang CJ, Lien RC. 2009. Prophylactic ureteral catheterization in gynecologic surgery: a 12-year randomized trial in a community hospital. Int Urogynecol J Pelvic Floor Dysfunct. 20: 689-693.[Ref.]
- Liapis A, Bakas P, Giannopoulos V, et al. 2001. Ureteral injuries during gynecological surgery. Int Urogynecol J Pelvic Floor Dysfunct. 12: 391-393.[Ref.]
- Patil SB, Guru N, Kundargi VS, et al. 2017. Posthysterectomy ureteric injuries: Presentation and outcome of management. Urol Ann. 9: 4-8.[Ref.]
- Satitniramai S, Manonai J. 2017. Urologic injuries during gynecologic surgery, a 10-year review. J Obstet Gynaecol Res. 43: 557-63.[Ref.]
- Neuman M, Eidelman A, Langer R, et al. 1991. Iatrogenic injuries to the ureter during gynecologic and obstetric operations. Surg Gynecol Obstet. 173: 268-272.[Ref.]
- Shaw J, Tunitsky-Bitton E, Barber MD, et al. 2014. Ureterovaginal fistula: a case series. Int Urogynecol J. 25: 615-621.[Ref.]
- Brandes S, Coburn M, Armenakas N, et al. 2004. Diagnosis and management of ureteric injury: an evidence-based analysis. BJU Int. 94: 277-289.[Ref.]
- Singh O, Gupta SS, Mathur RK. 2010. Urogenital fistulas in women: 5-year experience at a single center. Urol J. 7: 35-39.[Ref.]
- Sharp HT, Adelman MR. 2016. Prevention, Recognition, and Management of Urologic Injuries During Gynecologic Surgery. Obstet Gynecol. 127: 1085-1096.[Ref.]
- Siddighi S, Yune JJ, Hardesty J. 2014. Indocyanine green for intraoperative localization of ureter. Am J Obstet Gynecol. 211: 1-2.[Ref.]
- Dane B, Baxter AB, Bernstein MP. 2017. Imaging Genitourinary Trauma. Radiol Clin North Am. 55: 321-335.[Ref.]
- El-Tabey NA, Ali-El-Dein B, Shaaban AA, et al. 2006. Urological trauma after gynecological and obstetric surgeries. Scand J Urol Nephrol. 40: 225-231.[Ref.]
- Hulse CA, Sawtelle WW, Nadig PW, et al. 19968. Conservative management of ureterovaginal fistula. J Urol. 99: 42-49.[Ref.]
- Alonso Gorrea M, Fernandez Zuazu J, Mompo Sanchis JA, et al. 1986. Spontaneous healing of ureterogenital fistulas: selection criteria. Eur Urol. 12: 322-326.[Ref.]
- Elabd S, Ghoniem G, Elsharaby M, et al. 1997. Use of endoscopy in the management of postoperative ureterovaginal fistula. Int Urogynecol J Pelvic Floor Dysfunct. 8: 185-190.[Ref.]
- Kumar A, Goyal NK, Das SK, et al. 2009. Our experience with genitourinary fistulae. Urol Int. 82: 404-410.[Ref.]
- Al-Otaibi KM. 2012. Ureterovaginal fistulas: The role of endoscopy and a percutaneous approach. Urol Ann. 4: 102-105.[Ref.]
- Schmeller NT, Gottinger H, Schuller J, et al. 1983. [Percutaneous nephrostomy as primary therapy of ureterovaginal fistula]. Urologe A. 22: 108-112.[Ref.]
- Shelbaia AM, Hashish NM. 2007. Limited experience in early management of genitourinary tract fistulas. Urology. 69: 572-574.[Ref.]




















