Indexing & Abstracting
Full Text
Case ReportDOI Number : 10.36811/ijapr.2019.110002Article Views : 758Article Downloads : 27
Successful Treatment of medically refractory scleroderma digital gangrene with long-term continuous brachial plexus block
Marcoccia A1*, Salvucci C1, Di Carlo M2, Caravelli G3, Bosco M4 and Mazzini P5
1CRIIS, Scleroderma Referred Centre-Microvascular Unit-Sandro Pertini Hospital, Rome, Italy
2CRIIS, Scleroderma Referred Center-Pain Unit- Sandro pertini Hospital, Rome, Italy
3Dep, Plastic Surgery, S. Camillo Hospital, Rome, Italy
4Dep of Anesthesiology S. Spirito Hospital, Rome, Italy
5Dep of Anesthesiology S. Pertini Hospital, Rome, Italy
*Corresponding author: Marcoccia A, CRIIS, Scleroderma Referred Centre-Microvascular Unit-Sandro Pertini Hospital, Rome, Italy, Email: antonella.marcoccia@aslroma2.it
Article Information
Aritcle Type: Case Report
Citation: Marcoccia A, Salvucci C, Di Carlo M, et al. 2019. Successful Treatment of medically refractory scleroderma digital gangrene with long-term continuous brachial plexus block. Int J Anesthesi Pain Res. 1: 05-09.
Copyright:This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Copyright © 2019; Marcoccia A
Publication history:
Received date: 13 April, 2019Accepted date: 30 April, 2019
Published date: 02 May, 2019
Introduction
Raynaud’s phenomenon (RP) is the earliest and most common clinical manifestation of scleroderma, occurring in 90 to 98% of patients [1]. A combination of sympathetically mediated vasospasm and vasoocclusive disease has been implicated in the etiology of digital ischemic phenomenon [2,3], and treatment of RP is directed towards relieving vasospasm and restoring blood flow. Therefore, cervicothoracic or peripheral sympatholysis and digital artery reconstruction have been performed for medically refractory RP with scleroderma even though all procedures have some limitations. Thoracoscopic symapthectomy has recently been shown to have an initial improvement, although almost always relapses 6 months after the treatment [4,5]. Surgery of the hand, including digital sympathectomy and arterial reconstruction, for scleroderma might have favorable outcomes [6,7]. However, it would be a limited treatment option because of a recurrent ulcer after surgery [8], delayed wound healing [8,9], and development of complex regional pain syndrome [10]. Another alternative and less invasive treatment for blocking the sympathetic outflow would be a sympathetic block with local anesthetics [11,12]. These therapies are based on the premise that excessive sympathetic activity may be involved in the pathogenesis of digital ischemia.
Case Report
The Patients was diagnosed with diffuse systemic sclerosis nearly thirty years ago, diffuse cutaneous sclerosis, antitopoisomerasi-1 antibody (SCL-70) bilateral hands and feet Raynaud, past left forefoot amputation. She was treated with daily medications including long acting calcium channel blockers (nifedipine), oral endothelin -1 receptor inhibitor (bosentan), antiplatelets drug, proton pump inhibitor. The patient came to our observation complaining persistent Raynaud’s phenomenon with severe ischemic pain (VAS 9 -10). The angiogram was performed and revealed a distal ulnary obstructive lesions, radial segmental occlusion with reperfusion of the arch handheld by interosseous artery, narrowing of multiple digital arteries with a severe blood flow reduction due to vasospasm of digital arteries.

Medical therapy (iloprost, low molecular weight heparin, opioid) was started without benefit.
Small digital ulcers appeared and rapidly evolved in gangrene in a few weeks onto 2°, 3° and 4° finger of left hand despite medical therapy.

The pain is moderate during the day and worsen during the night with intensive pain peaks. She was treated with oxycodone, morphine, pregabalin doses high the skin temperature on her fingers was monitored at constant room temperature (21–22oC) with a skin temperature probe (TempTouch-infrared skin Thermometer- OPTIMA) 28-29 °C on left fingers and 31-32 °C on right fingers.
Methods
Considering the failure of medical treatment and the appearance, within few days, of necrosis in the distal , middle and in the prossimal phalanges of 3° and 4° finger, at first a diagnostic single shot axillary brachial plexus block with ropivacaine 0.375 30 ml was performed: the block showed immediate effectiveness with pain disappearance ( VAS 0) for 12 hours; the left hand also regained temperature 29-30 C and perfusion and return of interdigital flow revealed with continuous waves Doppler (CW). We decided then, with the aim of stopping the necrosis and limit ischemia and pain, given the monolateral pathology, to perform a continuous brachial plexus block.
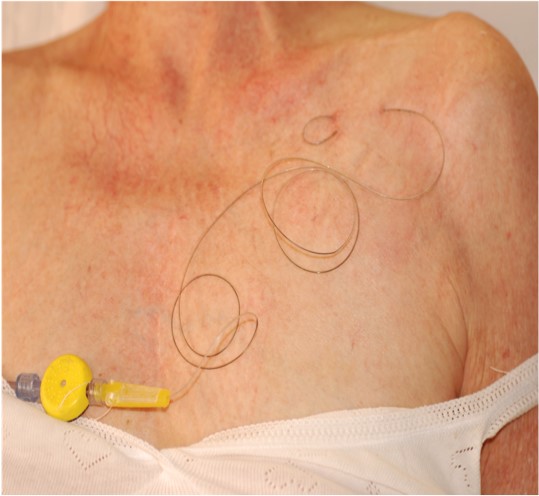
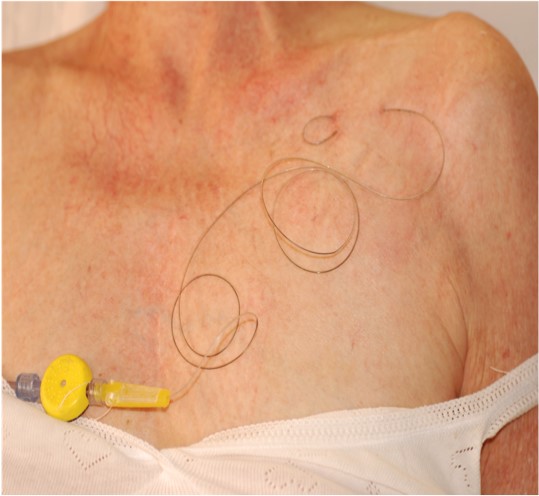
Considering a long-time treatment, we choose the infraclavicular approach for catheter positioning and the local anesthetic infusion. Infusion was started with Ropivacaine 0.2% 5 ml/hr and then reduced to 0.15% because of persistent and limitating motor block; at week 4 after block despite complete regression of algic symptoms (VAS 0), ischemia and termic gradient between right and left hand persisted.
So, a series of 4, weekly, stellate ganglion blocks were performed and continuous infusion of local anesthetic was continued with bupivacaine 0.125%. That allowed a demarcation of digital necrosis and the amputation of the distal phalanges of 3° and 4° finger was performed at week 9 after positioning.
Continuous infusion of Bupivacaine was continued allowing wound dressing and healing. We used continuous sympathetic block achieved through monolateral continuous long-term brachial plexus block instead of neuroablative sympathectomy in our patient to the fact that recurrence may occur at a high rate after thoracoscopic or chemically neurolytic sympathetomy [4,5,13,14]. Most patients with RP show initial improvement [5], however, all relapse 6 months after the thoracoscopic sympathectomy [4]. The high initial relief of symptoms and frequent recur-rence from neurorestorative sympathectomy might be caused by denervation super sensitivity or nerve re- generation [15,16]). After 18 weeks before removing perineural catheter and local anesthetic infusion the patients was treated with analgesic oral drugs (oxicodone 10/naloxone 5 mg, gabapentin 150x 3). When the anesthetic infusion was stopped the pain peak restarts (VAS 5) and the gabapentin was increased (300x3). About 2 months after catheter removal the healing process continued to improve and the pain was absent. Oxicodone /naloxone and gabapentin therapy were gradually reducted until final healing.
Results
On week 28 healing process was complete and pain absent (VAS 0); the hand appeared persistently warm and well perfused. Digital ulcers are completely healed without relapse until the last follow-up evaluation 3 years later on April 2017. The patient during brachial plexus block, showed an average 2 degrees increment of finger skin temperature at steady state compared to the baseline temperature. The skin temperature of left fingers increased from 28.5oC and 29oC at baseline mean temperature to 31oC and 32oC. Given a residual motor block, Bupivacaine infusion was reduced to 0.0625%, without any change in the clinical picture. Except for the time of surgery, the treatment was managed outpatient. Continuous long-term brachial plexus block can provide a significant effect on improving blood flow for wound healing of otherwise medically refractory upper limb gangrenous ulcer in patients with RP and systemic sclerosis.
Low dose and low concentration local anesthetic infusion allowed pain relief and improved peripheral perfusion, without motor block and minimal sensitive deficit. No toxicity and no catheter infections were observed. Except for the surgery, the patient's treatment has always been as outpatient. To our knowledge no other case was treated with such long-term brachial plexus block for ischemic pain and ulcers or other pathologic conditions caracterised by refractory pain.
Conclusion
Continuous infusion of local anesthetics achieved through monoliteral continuous long-term brachial plexus block can provide a significant effect on improving blood flow for wound healing of an otherwise medically refractory gangrenous ulcer of the fingertip in patients with Raynaud’s phenomenon and systemic sclerosis. However, more evidence is required to evaluate in patients with ischaemic ulcers the reliability of the continuous long-term brachial plexus block for effective sympatholysis. This is the first case report in literature of successful treatment of medically refractory scleroderma digital gangrene with long term continuous brachial plexus block for 18 weeks without any complication and with minimal local invasiveness, without relapse during 3 years of follow up.
References
- Bennett R, Bluestone R, Holt PJL, et al. 1971. Survival in scleroderma. Ann Rheum Dis. 30: 581-588. [Ref.]
- Miller LM, Morgan RF. 1993. Vasospastic dis- order: Etiology, recognition and treatment. Hand Clin 1993; 9:171-186. [Ref.]
- Rodnan GP, Myerowitz RL, Justh GO. 1980. Morphological changes in the digital arteries of patients with progressive systemic sclerosis (scleroderma) and Raynaud phenomenon. Medicine. 59: 393-408. [Ref.]
- Claes G, Drott C, Gothberg G. 1994. Thoracoscopic sympathicotomy for arterial insufficiency. Eur J Surg Suppl. 572: 63-64. [Ref.]
- Matsumoto Y, Ueyama T, Endo M, et al. 2002. Endoscopic thoracic sympathicotomy for Raynaud’s phenomenon. J Vasc Surg. 36: 57-61. [Ref.]
- Tomaina MM, Goitz RJ, Medsger TA. 2001. Surgery for ischemic pain and Raynaud’s phenomenon in scleroderma: A description of treatment protocol and evaluation of results. Microsurgery. 21: 75-79. [Ref.]
- Hafner J, Della Santa D, Zuber C, et al. 1997. Digital sympathectomy (microarteriolysis) in the treatment of severe Raynaud’s phenomenon secondary to systemic sclerosis. Br J Dermatol. 137: 1011-1031. [Ref.]
- Ward WA, Van Moore A. 1995. Management of finger ulcers in scleroderma. J Hand Surg (Am). 20: 868-872. [Ref.]
- Tham S, Grossman JAI. 1997. Limited micro- surgical arteriolysis for complication of digital vasospasm. J Hand Surg Br. 25: 611-613. [Ref.]
- Hafner J, Della Santa D, Zuber C, et al. 1997. Digital sympathectomy (microarteriolysis) in the treatment of severe Raynaud’s phenomenon secondary to systemic sclerosis. Br J Dermatol. 137: 1011-1031. [Ref.]
- Greengrass RA, Feinglass NG, Murray PM, et al. 2003. Continuous regional anesthesia before surgical peripheral sympathectomy in a patient with severe digital necrosis associated with Raynaud’s phenomenon and scleroderma. Reg Anesth Pain Med. 28: 354-358. [Ref.]
- Singelyn FJ, Seguy S, Gouverneur JM. 1999. Interscalene brachial plexus analgesia after open shoulder surgery: Continuous versus patient-controlled infusion. Anesth Analg. 89: 1216-1220. [Ref.]
- Mailis A, Meindok H, Papagapiou M, et al. 1994. Alterations of the three-phase bone scan after sympathectomy. The Clinical J of Pain. 10: 146-155. [Ref.]
- Baron R, Maier C. 1996. Reflex sympathetic dystrophy: Skin blood flow, sympathetic vasoconstrictor reflexes and pain before and after surgical sympathectormy. Pain. 67: 317-326. [Ref.]
- Guyton AC, Hall JE. 2000. Textbook of Medical Physiology. 10th edition. W.B. Saunders Company, Philadelphia. 705. [Ref.]
- Kyung Ream Han, Chan Kim, Eun Jung Park. 2008. Successful treatment of digital ulcers in a scleroderma patient with continuous bilateral thoracic sympathetic block. Pain Physician. 11: 91-96. [Ref.]




















